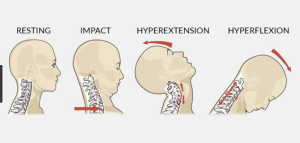
Acceleration/deceleration injury to the cervical spine(neck) and back, also known as whiplash, is a common injury due to traffic accidents regularly treated by our physiotherapists in Tralee. Whiplash as it is commonly known may result from rear-end or side impact motor collisions. It can also occur with activities such as diving or due to a direct blow from an opponent etc. The impact of any of these may result in injury to the cervical spine(bones of neck) or soft tissues such as the muscles or ligaments of the neck/back. This in turn leads to what is called ”whiplash associated disorders” or WAD for short(Spitzer, W.O., 1995).
To simplify the mechanism of this type of injury, think of a whip snapping. This is basically what is happening with your neck during these incidents, the head jolts swiftly forward first, then snaps backwards. It is being propelled swiftly with great force in one direction, then there is a recoil swiftly in the opposite direction. The back may also experience similar trauma.
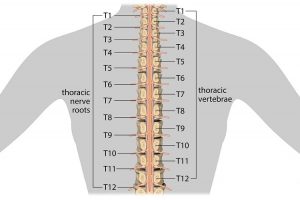
The most common symptoms of whiplash include neck pain, headache, back and shoulder pain with decreased mobility. The condition can be graded into WAD 1 – 4 depending on the degree on injury. With Wad 1 the patient complaints of pain, stiffness or tenderness only but no physical signs are noted. With Wad 2 the patient complains of neck pain and there is decreased range of motion and point tenderness in the neck. Where there are hard neurological signs, for example tingling and/or numbness down one or both arms WAD 3 is the grade assigned. Where there is a resulting fracture of the cervical spine, the term WAD 4 is used(Balla and Iansek, 1988, Stovner, L.J., 1996).
With whiplash the patient may not feel any pain immediately after the accident, however symptoms can increase gradually in the 48 hours after injury. Muscles, joints, ligaments and neural tissue can all be affected depending on the level of injury. Once an x-ray or Mri is performed to rule out serious injury to the bones, ligaments etc. of the neck , red flag signs also being ruled out, it is important that physical therapy is started as soon as possible. A multimodality approach to treatment as early as possible has shown good results in best evidence practice. This includes very specific therapeutic exercises, manual therapy, postural education and the use of drugs most notably non steroidal anti-inflammatories and muscle relaxants(Childs et al. 2008, 2009). It is extremely important to try to return range of movement to the neck as soon as possible after the accident once adequate safety checks have been performed. The neck stiffens up quite quickly when immobilized for even short periods of time. This current thinking is very different to years ago when neck braces and immobilization for long periods after accidents was standard.
Some symptoms associated with whiplash that can indicate the condition may be a little more serious, needing immediate review by a doctor or specialist include bilateral parasthesia(numbness on both sides of body), dizziness, feeling sick, a lump in throat when swollowing, progressively worsening neurological symptoms, signs of neck instability, unrelenting pain, increase in any of these symptoms with rotation or flexion of head. For more information on whiplash click here.
References
Balla J., Iansek, R., Headaches arising from disorders of the cervical spine. In : Hopkins A, ed. Headache. Problems in diagnosis and management. London: Saunders, 1988:241-67.
Childs, J.D., Cleland, J.A., Elliott, J.M. et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. Erratum appears in J. Orthop. Sports Phys. Ther. 2009 Apr;39(4):297, J. Orthop. Sports Phys. Ther. 2008;38(9):A1-34.
Spitzer, W.O., Skovron, M.L., Salami, L.R. et al. Scientific monograph of the Quebec Task Force on Whiplash Associated Disorders : redefining ”whiplash” and its management. Spine 1995;22(8suppl.):S1-73.
Stovner, L.J. The nosologic status of the whiplash syndrome: a critical review based on a methodological approach. Spine 1996; 21(23):2735-46.
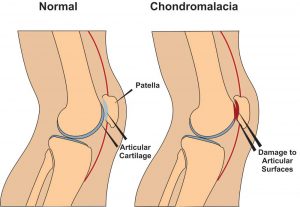 Chondromalacia patella, also known as ”Runners Knee” is one of the most common causes of knee pain in runners. The condition results from irritation of the cartilage on the under-surface of the kneecap. This cartilage is smooth and the kneecap normally glides effortlessly across it during bending of the knee joint. In some individuals however the kneecap does not track so smoothly due to poor alignment and the cartilage surface becomes irritated, resulting in inflammation and knee pain. In more severe cases there can be breakdown of the cartilage. Chondromalacia patella can affect athletes of any age but tends to be more common in women, most likely due to anatomical differences between the sexes ie. wider hips in females which results in a greater angulation between hip and knee, thus resulting in increased lateral forces on the patella.
Chondromalacia patella, also known as ”Runners Knee” is one of the most common causes of knee pain in runners. The condition results from irritation of the cartilage on the under-surface of the kneecap. This cartilage is smooth and the kneecap normally glides effortlessly across it during bending of the knee joint. In some individuals however the kneecap does not track so smoothly due to poor alignment and the cartilage surface becomes irritated, resulting in inflammation and knee pain. In more severe cases there can be breakdown of the cartilage. Chondromalacia patella can affect athletes of any age but tends to be more common in women, most likely due to anatomical differences between the sexes ie. wider hips in females which results in a greater angulation between hip and knee, thus resulting in increased lateral forces on the patella.
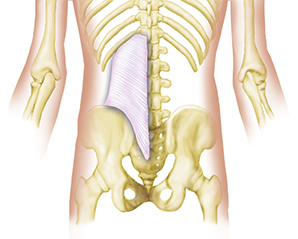
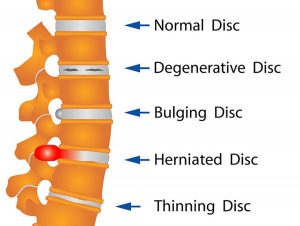 Your spine is made up of lots of bones called vertebrae and discs stacked on top of one another, forming the spinal canal. The nerves of the spinal cord run down the length of the spinal canal. The discs in act like shock absorbers between the vertebrae. These discs are made of two components: a softer center (called nucleus pulposus) surrounded by a tough elastic-like band (called annulus fibrosus). A bulging disc is like a squashed jam doughnut before the jam bursts out. The disc sags and looks like it is bulging outward. With a herniated disc, the outer covering of the disc has a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal. It is like the jam leaking out from the inside of a squashed jam doughnut.
Your spine is made up of lots of bones called vertebrae and discs stacked on top of one another, forming the spinal canal. The nerves of the spinal cord run down the length of the spinal canal. The discs in act like shock absorbers between the vertebrae. These discs are made of two components: a softer center (called nucleus pulposus) surrounded by a tough elastic-like band (called annulus fibrosus). A bulging disc is like a squashed jam doughnut before the jam bursts out. The disc sags and looks like it is bulging outward. With a herniated disc, the outer covering of the disc has a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal. It is like the jam leaking out from the inside of a squashed jam doughnut. Dry Needling
Dry Needling Spinal manipulation is a technique where practitioners use their hands or a device to apply a controlled thrust to a joint of your spine. The amount of force can vary, but the thrust moves the joint more than it would on its own. It is designed to relieve pressure on joints, reduce inflammation, and improve nerve function. It’s often used to treat back, neck, shoulder, and headache pain in combination with other treatments i.e. deep tissue massage, electrotherapy, rehabilitation exercises. The common goal of most spinal manipulations is to restore or to enhance joint function, with the general goals of resolving joint inflammation and reducing pain.
Spinal manipulation is a technique where practitioners use their hands or a device to apply a controlled thrust to a joint of your spine. The amount of force can vary, but the thrust moves the joint more than it would on its own. It is designed to relieve pressure on joints, reduce inflammation, and improve nerve function. It’s often used to treat back, neck, shoulder, and headache pain in combination with other treatments i.e. deep tissue massage, electrotherapy, rehabilitation exercises. The common goal of most spinal manipulations is to restore or to enhance joint function, with the general goals of resolving joint inflammation and reducing pain.