Overtraining syndrome, a common cause of persistent tiredness in sportspeople, seen by physio’s, frequently occurs in athletes who are training for competition or a specific event and train beyond their bodies ability to recover. Athletes often exercise longer and harder so that they can improve. However without adequate rest, recovery and nutrition, these training regimens can backfire, actually decreasing performance. Proper training and conditioning requires a balance between overload and recovery. The terms overtraining, overreaching, overtraining syndrome, burnout, and staleness have all been associated with overtraining syndrome and need to be clarified. Overtraining is excessive training with inadequate recovery. Overtraining has also been linked to glycogen depletion(Costill et al. 1988) when inadequate refuelling of muscles glycogen occurs due to low carbohydrate intake. The sooner carbohydrate is consumed following a bout of exercise, the more effective the replenishment of glycogen stores. Adequate quality protein intake would also be important in the case of strength athletes to help protect against overtraining syndrome. Sufficient iron intake is important for endurance athletes especially women.
Overtraining syndrome, a common cause of persistent tiredness in sportspeople, seen by physio’s, frequently occurs in athletes who are training for competition or a specific event and train beyond their bodies ability to recover. Athletes often exercise longer and harder so that they can improve. However without adequate rest, recovery and nutrition, these training regimens can backfire, actually decreasing performance. Proper training and conditioning requires a balance between overload and recovery. The terms overtraining, overreaching, overtraining syndrome, burnout, and staleness have all been associated with overtraining syndrome and need to be clarified. Overtraining is excessive training with inadequate recovery. Overtraining has also been linked to glycogen depletion(Costill et al. 1988) when inadequate refuelling of muscles glycogen occurs due to low carbohydrate intake. The sooner carbohydrate is consumed following a bout of exercise, the more effective the replenishment of glycogen stores. Adequate quality protein intake would also be important in the case of strength athletes to help protect against overtraining syndrome. Sufficient iron intake is important for endurance athletes especially women.
The term overreaching describes similar symptoms(fatigue, performance decrements, mood state
changes) but is generally of a more transitory nature and is often utilised by sportspeople/coaches
during a typical training cycle to enhance performance. Intense training, in the short term can result
in a decline in performance; however when incorporated with periods of recovery, a
super-compensation effect may occur, with the sportsperson exhibiting enhanced performance
when compared with baseline level (Halson and Jeukendrup, 2004). Overtraining syndrome
develops when there is failed adaptation to overload training due to inadequate regeneration.
Unfortunately , many sportspeople and coaches, especially at amateur level, react to impaired
performance by increasing the intensity of training. This leads to further impairment of
performance, which may , in turn, result in the sportsperson increasing training even further. A
vicious cycle develops which leads overtraining syndrome.
Changes within the central nervous system seem to play an important role in the development of
chronic fatigue and many of the other common signs and symptoms that are frequently seen in
overtraining syndrome, such as disrupted sleep, changes in appetite and weight, irritability, impaired
concentration, decreased motivation, and depressed mood. It has been suggested that alterations in
levels of brain neurotransmitters(e.g. a reduction in serotonin levels) and an increased release of
inflammatory mediators(e.g. cytokines) are important factors in the development of overtraining
syndrome(Anish, 2005). Many of the signs and symptoms that characterize overtraining syndrome are remarkably similar to those of clinical depression. Unfortunately, no single test can detect overtraining in the sportsperson. Probably the simplest and most effective means of monitoring overtraining is self analysis by sportspeople themselves. Daily documentation should include sources and ratings of stress, fatigue, muscle soreness, quality of sleep, irritability, and perceived exertion during training or standardized exercise.
Blood parameters such as red and white blood cell counts, haemoglobin, hematocrit, urea, and
ammonia are usually normal during overtraining. Changes in exercise blood lactate concentration
and blood lactate threshold however have been shown to be good indicators of overtraining but are
influenced by many other factors and are probably only useful if assessed repeatedly.
The initial symptom of the overtraining syndrome is usually fatigue but in time, other symptoms
develop.(Mackinnon and Hooper, 2000) Indicators of overtraining include; decreased performance
despite continued training, persistent fatigue, increased early morning heart rate or resting blood
pressure, frequent illnesses such as upper respiratory tract infections, persistent muscle soreness,
loss of body mass, mood changes, loss of appetite, sleep disturbance, high self-reported stress
levels, irritability, depression , decreased maximal heart rate. Overtraining syndrome can also leave
an athlete more susceptible to injury.
Deep tissue massage and injury prevention advice is where or physiotherapists come in. Feel free to set up an appointment at our Tralee clinic to discuss things. For more details click here.
REFERENCES
Anish, E.J. Exercise and its effects on the central nervous system. Curr. Sports Med. Rep. 2005:4:18-23.
Costill, D.L., Flynn, M.G., Kirwan, J.P. et al. Effects of repeated days of intensified training on muscle glycogen and swimming performance. Med. Sci. Sports Exerc. 1988;20:249-54.
Halson, S.L., Jeukendrup, A.E.https://pubmed.ncbi.nlm.nih.gov/15571428/ Does overtraining exist? An analysis of overreaching and overtraining research. Sports Med. 2004;34(14):967-81.
Mackinnon, L.T., Hooper, S.L. Overtraining and overrreaching: causes, effects, and prevention. In :
Garret, W.E., Kirkendall, D.T., eds. Exercise and Sports Science. Philadelphia : Lippincott, William &
Wilkins, 2000.
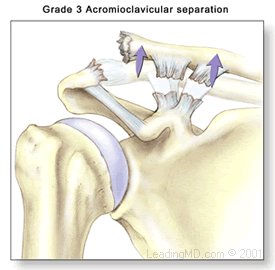
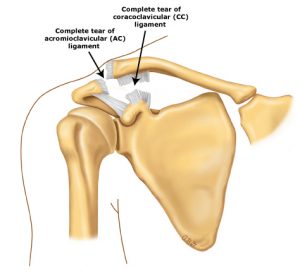 AC joint separation injuries are dislocations of the clavicle from the acromion. The severity of these depends on which supporting structures are damaged, and the extent of that damage. Tearing of the acromioclavicular ligament alone is not a serious injury, but when the coracoclavicular ligaments are ruptured, the result is major instability in the shoulder area.
AC joint separation injuries are dislocations of the clavicle from the acromion. The severity of these depends on which supporting structures are damaged, and the extent of that damage. Tearing of the acromioclavicular ligament alone is not a serious injury, but when the coracoclavicular ligaments are ruptured, the result is major instability in the shoulder area.
 Overtraining syndrome, a common cause of persistent tiredness in sportspeople, seen by physio’s, frequently occurs in athletes who are training for competition or a specific event and train beyond their bodies ability to recover. Athletes often exercise longer and harder so that they can improve. However without adequate rest, recovery and nutrition, these training regimens can backfire, actually decreasing performance. Proper training and conditioning requires a balance between overload and recovery. The terms overtraining, overreaching, overtraining syndrome, burnout, and staleness have all been associated with overtraining syndrome and need to be clarified. Overtraining is excessive training with inadequate recovery. Overtraining has also been linked to glycogen depletion(Costill et al. 1988) when inadequate refuelling of muscles glycogen occurs due to low carbohydrate intake. The sooner carbohydrate is consumed following a bout of exercise, the more effective the replenishment of glycogen stores. Adequate quality protein intake would also be important in the case of strength athletes to help protect against overtraining syndrome. Sufficient iron intake is important for endurance athletes especially women.
Overtraining syndrome, a common cause of persistent tiredness in sportspeople, seen by physio’s, frequently occurs in athletes who are training for competition or a specific event and train beyond their bodies ability to recover. Athletes often exercise longer and harder so that they can improve. However without adequate rest, recovery and nutrition, these training regimens can backfire, actually decreasing performance. Proper training and conditioning requires a balance between overload and recovery. The terms overtraining, overreaching, overtraining syndrome, burnout, and staleness have all been associated with overtraining syndrome and need to be clarified. Overtraining is excessive training with inadequate recovery. Overtraining has also been linked to glycogen depletion(Costill et al. 1988) when inadequate refuelling of muscles glycogen occurs due to low carbohydrate intake. The sooner carbohydrate is consumed following a bout of exercise, the more effective the replenishment of glycogen stores. Adequate quality protein intake would also be important in the case of strength athletes to help protect against overtraining syndrome. Sufficient iron intake is important for endurance athletes especially women.
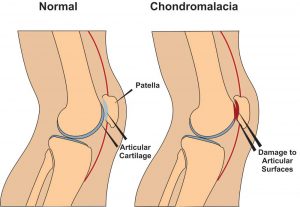 Chondromalacia patella, also known as ”Runners Knee” is one of the most common causes of knee pain in runners. The condition results from irritation of the cartilage on the under-surface of the kneecap. This cartilage is smooth and the kneecap normally glides effortlessly across it during bending of the knee joint. In some individuals however the kneecap does not track so smoothly due to poor alignment and the cartilage surface becomes irritated, resulting in inflammation and knee pain. In more severe cases there can be breakdown of the cartilage. Chondromalacia patella can affect athletes of any age but tends to be more common in women, most likely due to anatomical differences between the sexes ie. wider hips in females which results in a greater angulation between hip and knee, thus resulting in increased lateral forces on the patella.
Chondromalacia patella, also known as ”Runners Knee” is one of the most common causes of knee pain in runners. The condition results from irritation of the cartilage on the under-surface of the kneecap. This cartilage is smooth and the kneecap normally glides effortlessly across it during bending of the knee joint. In some individuals however the kneecap does not track so smoothly due to poor alignment and the cartilage surface becomes irritated, resulting in inflammation and knee pain. In more severe cases there can be breakdown of the cartilage. Chondromalacia patella can affect athletes of any age but tends to be more common in women, most likely due to anatomical differences between the sexes ie. wider hips in females which results in a greater angulation between hip and knee, thus resulting in increased lateral forces on the patella.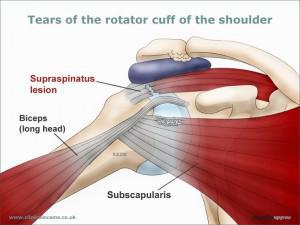
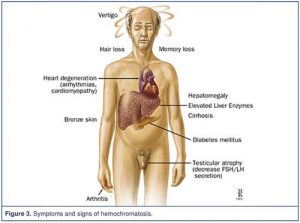 Haemochromatosis is a inherited condition where iron levels in the body increase over many years leading to iron overload. If the condition is not treated, it can lead to damage in certain parts of the
Haemochromatosis is a inherited condition where iron levels in the body increase over many years leading to iron overload. If the condition is not treated, it can lead to damage in certain parts of the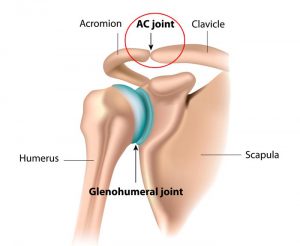 AC joint injuries occur where the acromion connects to the clavicle on the top of the shoulder. This joint helps maintain the position of the shoulder and is very important for shoulder control, motion, and strength. The joint is stabilized by a capsule and ligaments. Injury occurs when these structures get damaged. If severe the injury can lead to joint instability and pain. These type of injuries are usually the result of a sudden fall onto the shoulder. The AC joint is also a common place for arthritis to develop. This is usually the result of years of “wear and tear” on the joint and is common in weight lifters and laborers.
AC joint injuries occur where the acromion connects to the clavicle on the top of the shoulder. This joint helps maintain the position of the shoulder and is very important for shoulder control, motion, and strength. The joint is stabilized by a capsule and ligaments. Injury occurs when these structures get damaged. If severe the injury can lead to joint instability and pain. These type of injuries are usually the result of a sudden fall onto the shoulder. The AC joint is also a common place for arthritis to develop. This is usually the result of years of “wear and tear” on the joint and is common in weight lifters and laborers.