Lumbosacral Plexopathy : Recently I had a patient present with footdrop (foot drops and drags as you walk due to weakness in dorsiflexor muscles), also severe pain down the leg, along with lumbar-sacral pain(lower back area). Initially this might appear to be signs of disc herniation with nerve root compression, even though the footdrop would be fairly uncommon with that condition. An MRI showed the spine to be normal. We also looked at anything that might have injured the peroneal nerve which is quiet close to the skin on the lower leg, which in itself could cause the footdrop, but there was no sign of injury. We were also able to rule out diabetes which can lead to nerve damage.
So where did we go next? Answer : An electromyography (EMG)(nerve conduction study). Electromyography is a diagnostic procedure used to assess the health of muscles and the nerve cells that control them (motor neurons). EMG results can reveal nerve dysfunction, muscle dysfunction or problems with nerve-to-muscle signal transmission. As a result of this testing by a specialist, the client was diagnosed as having a Lumbosacral plexopathy. In this case it seemed that the nerve had been damaged by a viral or bacterial infection. More tests need to be done to confirm and treat this infection.
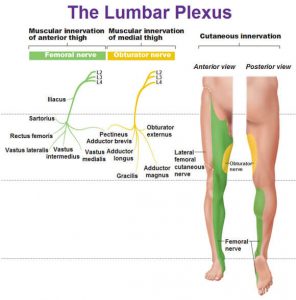
The lumbosacral plexus represents the nerve supply to the lower back, pelvis and legs. Lumbosacral plexopathy is characterized as inflammation and or damage to the nerve bundles in the area of the lumbar and sacral vertebrae regions. Symptoms may include shooting or burning pain, numbness, and decreased movement in the thigh, buttock and/or leg area. It is an uncommon idiopathic disorder(relates to or denotes any disease or condition which arises spontaneously or for which the cause is unknown). It is characterized by the acute onset of severe lower extremity pain followed by wasting and weakness of leg muscles along with variable sensory loss.
To Summarise : Lower Lumbosacral Plexopathy
It predominantly affect the L4–S3 nerve fibers.
There patient complains of a deep boring pain in the pelvis that can radiate posteriorly into the thigh and down into the posterior and lateral calf.
The ankle reflex may be depressed or absent.
Sensory symptoms and signs may be severely deminished over the posterior thigh and posterior-lateral calf and in the foot.
Other Causes of Lumbosacral Plexopathy
Structural
Retroperitoneal hemorrhage (anticoagulation, hemophilia)
Pelvic or abdominal tumor
Aneurysm (common or internal iliac artery)
Endometriosis
Trauma
Nonstructural
Inflammatory (plexitis)
Infarction
Postpartum [during childbirth]
Diabetes (diabetic amyotrophy – most common non-structural cause)
Radiation
Postsurgical (retractor injury)
Please note that the presentation of Lumbosacral Plexopathy has subtle differences to sciatica and discogenic pain, the later conditions being much more common than Lumbosacral Plexopathy.
Physiotherapists in Tralee Phone 086-7700191 to discuss your condition or to make an appointment.
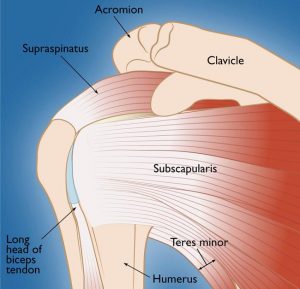 Rotator Cuff Tears
Rotator Cuff Tears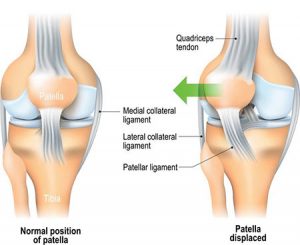 Knee injuries like Chondromalacia patella result from degeneration of cartilage on the underside the kneecap (patella)due to poor alignment of the kneecap (patella) as it slides over the lower end of the thighbone (femur). This condition can also be referred to as patellofemoral syndrome. It usually presents as pain in the front of the knee aggravated by activities such as running, jumping, climbing or descending stairs etc., or by prolonged sitting with knees in a moderately bent position. Patients with chondromalacia patella frequently have abnormal patellar “tracking” toward the lateral (outer) side of the femur. Some patients may also have a vague sense of “tightness” or “fullness” in the knee area with the condition. Mild swelling of the knee area may also occur.
Knee injuries like Chondromalacia patella result from degeneration of cartilage on the underside the kneecap (patella)due to poor alignment of the kneecap (patella) as it slides over the lower end of the thighbone (femur). This condition can also be referred to as patellofemoral syndrome. It usually presents as pain in the front of the knee aggravated by activities such as running, jumping, climbing or descending stairs etc., or by prolonged sitting with knees in a moderately bent position. Patients with chondromalacia patella frequently have abnormal patellar “tracking” toward the lateral (outer) side of the femur. Some patients may also have a vague sense of “tightness” or “fullness” in the knee area with the condition. Mild swelling of the knee area may also occur.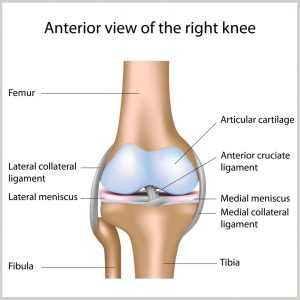 Any activity that causes you to forcefully twist or rotate your knee, especially when putting your full weight on it, can lead to a torn meniscus. Each of your knees has two menisci — C-shaped pieces of cartilage that act like a cushion between your shinbone and your thighbone. A torn meniscus causes pain, swelling and stiffness. You might also feel your knee lock and have trouble extending it fully. Conservative treatment — such as rest, ice and medication — is sometimes enough to relieve the pain of a torn meniscus and allow the injury time to settle down on its own. In other cases, however, a torn meniscus requires surgical repair.
Any activity that causes you to forcefully twist or rotate your knee, especially when putting your full weight on it, can lead to a torn meniscus. Each of your knees has two menisci — C-shaped pieces of cartilage that act like a cushion between your shinbone and your thighbone. A torn meniscus causes pain, swelling and stiffness. You might also feel your knee lock and have trouble extending it fully. Conservative treatment — such as rest, ice and medication — is sometimes enough to relieve the pain of a torn meniscus and allow the injury time to settle down on its own. In other cases, however, a torn meniscus requires surgical repair.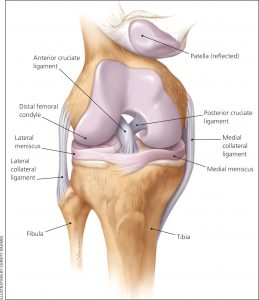 These ligaments are found inside your knee joint. They cross each other to form an “X” with the anterior cruciate ligament in front and the posterior cruciate ligament in back. The cruciate ligaments stabilize the knee. About half of all injuries to the anterior cruciate ligament occur along with damage to other structures of the knee, such as articular cartilage, meniscus, or other ligaments. Partial tears of the anterior cruciate ligament are rare; most ACL injuries are complete or near complete tears.
These ligaments are found inside your knee joint. They cross each other to form an “X” with the anterior cruciate ligament in front and the posterior cruciate ligament in back. The cruciate ligaments stabilize the knee. About half of all injuries to the anterior cruciate ligament occur along with damage to other structures of the knee, such as articular cartilage, meniscus, or other ligaments. Partial tears of the anterior cruciate ligament are rare; most ACL injuries are complete or near complete tears.
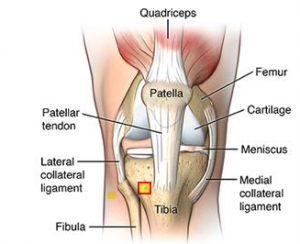 Patellar tendinopathy(also known as Jumper’s knee) is an overuse injury affecting this knee tendon. There are a number of factors which can contribute to the development of patellar tendinopathies. These include:
Patellar tendinopathy(also known as Jumper’s knee) is an overuse injury affecting this knee tendon. There are a number of factors which can contribute to the development of patellar tendinopathies. These include: Osgood-Schlatter disease is a common cause of knee pain in growing adolescents. It is an inflammation of the area just below the knee where the tendon from the kneecap (patellar tendon) attaches to the shinbone (tibia) called the tibial tuberosity. The condition gets worse with activity and better with rest. Osgood-Schlatter disease most often occurs during growth spurts, when bones, muscles, tendons, and other structures are changing rapidly. Because physical activity puts additional stress on bones and muscles, children who participate in athletics — especially running and jumping sports – are at an increased risk for this condition. However, less active adolescents may also experience this problem. The condition normally resolves over time but can be anything from a few weeks/months to two years. It is nothing to worry about. A child can remain active but pain from the condition itself will limit that activity. Icing the area of pain and stretching leg muscles especially quads can help. NSAIDs can be used to relief the pain and inflammation but should be used sparingly and under doctors supervision.
Osgood-Schlatter disease is a common cause of knee pain in growing adolescents. It is an inflammation of the area just below the knee where the tendon from the kneecap (patellar tendon) attaches to the shinbone (tibia) called the tibial tuberosity. The condition gets worse with activity and better with rest. Osgood-Schlatter disease most often occurs during growth spurts, when bones, muscles, tendons, and other structures are changing rapidly. Because physical activity puts additional stress on bones and muscles, children who participate in athletics — especially running and jumping sports – are at an increased risk for this condition. However, less active adolescents may also experience this problem. The condition normally resolves over time but can be anything from a few weeks/months to two years. It is nothing to worry about. A child can remain active but pain from the condition itself will limit that activity. Icing the area of pain and stretching leg muscles especially quads can help. NSAIDs can be used to relief the pain and inflammation but should be used sparingly and under doctors supervision.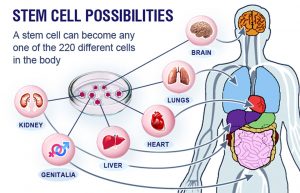 Recently in Ireland, people are paying thousands of euro for procedures advertised as ” stem cell treatment ”, for conditions such as osteoarthritis. These treatments are not covered by health insurance companies etc. They often use the term ”stem cell treatment”, for a process that bears little if any resemblance to what stem cell therapy actually is. Below is a summary of an article written by an orthopedic surgeon outlining the limitations of stem cell therapy as it presently stands. Before you part with your money for one of these treatments, have a read of it, discuss it with your doctor and do your research.
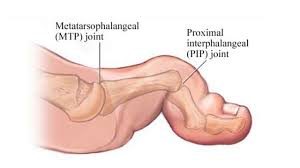
Recently in Ireland, people are paying thousands of euro for procedures advertised as ” stem cell treatment ”, for conditions such as osteoarthritis. These treatments are not covered by health insurance companies etc. They often use the term ”stem cell treatment”, for a process that bears little if any resemblance to what stem cell therapy actually is. Below is a summary of an article written by an orthopedic surgeon outlining the limitations of stem cell therapy as it presently stands. Before you part with your money for one of these treatments, have a read of it, discuss it with your doctor and do your research.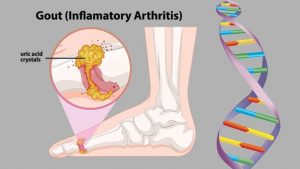 Gout is a form of arthritis which starts as a result of excess uric acid build-up in the blood, also called hyperuricemia. It is an extremely painful condition. Uric acid is produced in the body during the breakdown of purines – chemical compounds that are found in certain foods such as meat, poultry, and seafood. Normally, uric acid is dissolved in the blood and is excreted from the body in the urine via the kidneys. If too much uric acid is produced, it can build up and form needle-like crystals that trigger inflammation and pain in the joints and surrounding tissue. The condition often starts by affecting the joint at the base of the big toe. Attacks often occur without warning and in the middle of the night. They can come on quickly and keep returning over time, slowly damaging tissues in the region of the inflammation.
Gout is a form of arthritis which starts as a result of excess uric acid build-up in the blood, also called hyperuricemia. It is an extremely painful condition. Uric acid is produced in the body during the breakdown of purines – chemical compounds that are found in certain foods such as meat, poultry, and seafood. Normally, uric acid is dissolved in the blood and is excreted from the body in the urine via the kidneys. If too much uric acid is produced, it can build up and form needle-like crystals that trigger inflammation and pain in the joints and surrounding tissue. The condition often starts by affecting the joint at the base of the big toe. Attacks often occur without warning and in the middle of the night. They can come on quickly and keep returning over time, slowly damaging tissues in the region of the inflammation.
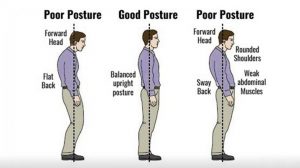 The increasing time we are spending glued to our phones or in front of a laptop with poor posture is manifesting itself with a
The increasing time we are spending glued to our phones or in front of a laptop with poor posture is manifesting itself with a 
 Spinal stenosis is a narrowing of the space within the spine. This can put pressure on the nerves that travel through the spine. It occurs most often in the lower back and the neck. Some people are born with a congenital form, but most develop it as part of the degenerative cascade. Sometimes people do not feel effects of the narrowing, but as part of the aging process, most people will eventually notice radiating pain, weakness, and/or numbness secondary to the compression of the nerves or spinal cord. In lumbar stenosis, the spinal nerve roots in the lower back become compressed and this can produce – tingling, weakness or numbness that radiates from the low back and into the buttocks and legs, especially with activity.
Spinal stenosis is a narrowing of the space within the spine. This can put pressure on the nerves that travel through the spine. It occurs most often in the lower back and the neck. Some people are born with a congenital form, but most develop it as part of the degenerative cascade. Sometimes people do not feel effects of the narrowing, but as part of the aging process, most people will eventually notice radiating pain, weakness, and/or numbness secondary to the compression of the nerves or spinal cord. In lumbar stenosis, the spinal nerve roots in the lower back become compressed and this can produce – tingling, weakness or numbness that radiates from the low back and into the buttocks and legs, especially with activity.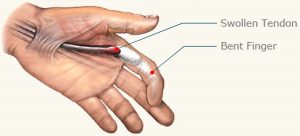 Trigger finger is a condition in which one of your fingers gets stuck in a bent position. Your finger may bend or straighten with a snap — like a trigger being pulled and released.
Trigger finger is a condition in which one of your fingers gets stuck in a bent position. Your finger may bend or straighten with a snap — like a trigger being pulled and released.