Muscle Tear or Spasm ? Which is it ?
 When somebody first presents in clinic with a muscle injury, it is important to first determine whether it is a muscle spasm or a tear. A spasm/cramp can often be worked out in a session with deep tissue massage and maybe some dry needling and stretching, allowing almost immediate turn to training. A muscle tear takes much longer to recover from, the length of time greatly depending on the degree of tearing. Treatment takes longer and a rehabilitation program is also essential. A muscle spasm is caused by an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time.
When somebody first presents in clinic with a muscle injury, it is important to first determine whether it is a muscle spasm or a tear. A spasm/cramp can often be worked out in a session with deep tissue massage and maybe some dry needling and stretching, allowing almost immediate turn to training. A muscle tear takes much longer to recover from, the length of time greatly depending on the degree of tearing. Treatment takes longer and a rehabilitation program is also essential. A muscle spasm is caused by an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time.
What is a Spasm?
A muscle spasm is an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time.
Spasm Causes
Spasms are usually caused by problems such as overworking a muscle, poor hydration, electrolyte imbalances, insufficient blood flow to the muscle or nerve compression. A pulled muscle is actually a tear in the muscle tissue. This occurs when the muscle is strained to the point where the muscle is damaged. The more significant the strain, the more the muscle can be torn.
What is a Muscle pull/Tear?
A pulled muscle is actually a tear in the muscle tissue. This occurs when the muscle is strained to the point where the muscle is damaged. The more significant the strain, the more the muscle can be torn.Pulled muscles are usually the result of not preparing the muscle for work through proper stretching, placing too much tension on the muscle or over-using the muscle. Soreness in the affected muscle is usually the first symptom. Using the muscle will be painful and difficult. In severe pulls, bruising may be present. The affected muscle will become very tender to the touch and some swelling may occur.
Pulled Muscle Causes
Pulled muscles are usually the result of one or a combination of (1) not preparing the muscle for work because of insufficient warmup,(2) lack of a proper stretching program after training to help the muscle recover,(3) placing too much tension on the muscle all of a sudden, (4) or over-using the muscle. Sharp pain in the affected muscle is usually the first symptom. Using the muscle will be painful and difficult. In severe pulls, bruising may be present. The affected muscle will become very tender to the touch and some swelling may occur.
The use of anabolic steroids is frequently linked to severe muscle tears as the body hasn’t had time to adapt to the increased workload . All training needs gradual progression and enough recovery time after training. The higher the intensity in training , the more time needed to recover. So for an athlete, periods of maximal performance require more recovery time.
For treatment of muscle tears or spasms phone 086-7700191. We are physiotherapists in Tralee.
 One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
 cartilage can be damaged by injury or normal wear and tear.
cartilage can be damaged by injury or normal wear and tear.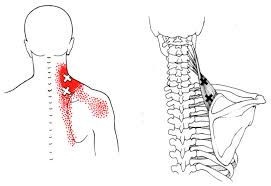

 Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
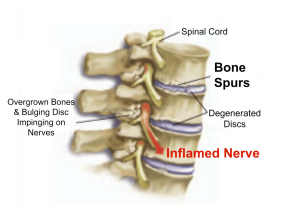 Bone spurs may or may not cause symptoms. Symptoms are location dependent. If bone spurs rub against other bones at joints they can cause pain and/or more limited movement in these joints. They can also be associated with pain, numbness, tenderness, and /or weakness in areas where they irritate adjacent tissue structures(muscles, ligaments, bones, nerves etc.). If the bone spur rubs against tendons or ligaments, they can sometimes cause a tear in these tissues over time. This is a common cause of tears in certain rotator cuff tendons .
Bone spurs may or may not cause symptoms. Symptoms are location dependent. If bone spurs rub against other bones at joints they can cause pain and/or more limited movement in these joints. They can also be associated with pain, numbness, tenderness, and /or weakness in areas where they irritate adjacent tissue structures(muscles, ligaments, bones, nerves etc.). If the bone spur rubs against tendons or ligaments, they can sometimes cause a tear in these tissues over time. This is a common cause of tears in certain rotator cuff tendons .
 A ”dead leg”, also known as ”charley horse” or ”quadriceps contusion”, is essentially an injury due to a traumatic blow, crushing the quadriceps muscle against the femur bone. The quadriceps is the muscle at the front of your thigh. The injury can be either intermuscular or intramuscular. Treatment depends on the type of contusion and grade in severity of the injury. An Intramuscular contusion occurs when the muscle gets torn within the sheath surrounding it. This causes the initial bleeding to cease within hours due to increased pressure within the muscle. However, the fluid and blood is not able to escape from the muscle sheath surrounding it resulting in considerable loss of function and a lot of pain. This can take days or weeks for a full recovery. You are unlikely to see any bruising with this type of contusion, especially in the early stages. In the case of intermuscular contusions, the muscle as well as part of the sheath surrounding it gets torn. This results in a longer bleeding time initially, especially if there is no use of ice therapy. The patient usually recovers faster from this type of dead leg, as the blood and fluids can easily flow away from the injury site. Bruising is often present in this type of contusion.
A ”dead leg”, also known as ”charley horse” or ”quadriceps contusion”, is essentially an injury due to a traumatic blow, crushing the quadriceps muscle against the femur bone. The quadriceps is the muscle at the front of your thigh. The injury can be either intermuscular or intramuscular. Treatment depends on the type of contusion and grade in severity of the injury. An Intramuscular contusion occurs when the muscle gets torn within the sheath surrounding it. This causes the initial bleeding to cease within hours due to increased pressure within the muscle. However, the fluid and blood is not able to escape from the muscle sheath surrounding it resulting in considerable loss of function and a lot of pain. This can take days or weeks for a full recovery. You are unlikely to see any bruising with this type of contusion, especially in the early stages. In the case of intermuscular contusions, the muscle as well as part of the sheath surrounding it gets torn. This results in a longer bleeding time initially, especially if there is no use of ice therapy. The patient usually recovers faster from this type of dead leg, as the blood and fluids can easily flow away from the injury site. Bruising is often present in this type of contusion.
