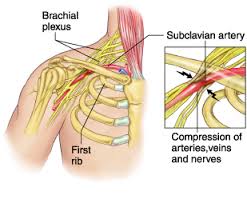
 Thoracic outlet syndrome is a disorder that occurs when the blood vessels or nerves in the space between the collarbone and first rib (thoracic outlet) become compressed. This can result in any of the following symptoms ; 1. pain in your shoulders and/or neck , 2. numbness / pain / tingling down the arm and / or in a finger / fingers. Common causes include physical trauma, i.e. car crash ; repetitive injuries from job or sports related activities; anatomical defects (such as having an extra rib); poor posture( protruding neck / rounded shoulders); and pregnancy.
Thoracic outlet syndrome is a disorder that occurs when the blood vessels or nerves in the space between the collarbone and first rib (thoracic outlet) become compressed. This can result in any of the following symptoms ; 1. pain in your shoulders and/or neck , 2. numbness / pain / tingling down the arm and / or in a finger / fingers. Common causes include physical trauma, i.e. car crash ; repetitive injuries from job or sports related activities; anatomical defects (such as having an extra rib); poor posture( protruding neck / rounded shoulders); and pregnancy.
You may notice symptoms of thoracic outlet syndrome if your job requires you to do a repetitive movement continuously for long periods, i.e. typing on a computer; working on an assembly line; or lifting things above your head. These repetitive activities tend to tighten up neck and shoulder muscles. Athletes, such as baseball pitchers and swimmers can also develop thoracic outlet syndrome from the years of repetitive movements.
Obesity can put an undue amount of stress on your body structures and joints leading to the development of thoracic outlet syndrome. Carrying around an over sized bag or backpack or having somebody sitting on your shoulders for long periods, say at a concert can compress nerve structures etc. and lead to the condition. You may suffer symptoms during pregnancy as muscles, ligaments, tendons and joints come under strain. This is as a result of the release of the hormone relaxin around week twelve of pregnancy, and also due to the increase in bodyweight.
The two most common types of thoracic outlet syndrome are:
1. Neurogenic (neurological) : This form of thoracic outlet syndrome is characterized by compression of the brachial plexus ( nerves coming from the spinal cord (neck). This network of nerves controls muscle movements and sensations in the shoulder, arm and hand. This is the most common cause of thoracic outlet syndrome.
Signs and symptoms include:
• Numbness or tingling in your arm or fingers.
• Wasting of muscles through which the compressed nerve travels; either in the arm or fingers or both.
• Pain in the neck , shoulder or hand.
• Weakened grip in hand / loss of strength in the arm.
Treatment : Often if neurogenic thoracic outlet syndrome is caught early, deep tissue work on neck, shoulders and arm to loosen out tightened muscles; joint mobilisations / manipulation of the cervical and thoracic spine; electro acupuncture along the affected nerve pathway; postural correction exercises, can usually bring great relief within one or two treatment sessions. If the condition is chronic ( i.e. there a month or months), it may take more time for the irritated nerve to settle. You may need to lose weight if obesity is the cause of your thoracic outlet syndrome.
2.Vascular (venous or arterial): This type occurs when one or more of the veins or arteries are compressed in the area between the collarbone and first rib.
Signs and symptoms include:
• Discoloration of the hand (bluish colour).
• Arm pain and swelling, possibly due to blood clots.
• Blood clots in veins or arteries in the upper area of your body.
• Lack of colour in one or more of your fingers or your entire hand.
• Weakened or no pulse in the affected arm.
• Cold fingers, hands or arms.
• Arm fatigue after activity.
• Numbness or tingling in your fingers.
• Throbbing lump near your collar bone.
• Weakness of arm or neck.
Treatment : For vascular (venous or arterial) thoracic outlet syndrome…you need to consult with your doctor. This condition may require thrombolytic medications, anticoagulant medications or surgery.


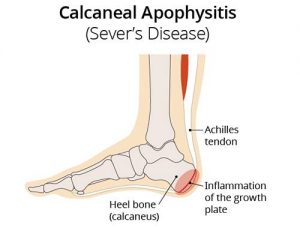 Sever’s disease (also known as calcaneal apophysitis) is a type of bone injury in kids whre the growth plate on the lower back part of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and painful. The reason for this is that the heel bone grows faster than the ligaments in the leg. As a result, muscles and tendons can become very tight and overstretched in children who are going through growth spurts. Sever’s disease occurs as a result of repetitive stress on the Achilles tendon. Over time, constant pressure on the already tight achilles tendon can damage the growth plate, causing children. Symptoms of Severs disease include pain and inflammation. This is why it is more common in physically active.
Sever’s disease (also known as calcaneal apophysitis) is a type of bone injury in kids whre the growth plate on the lower back part of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and painful. The reason for this is that the heel bone grows faster than the ligaments in the leg. As a result, muscles and tendons can become very tight and overstretched in children who are going through growth spurts. Sever’s disease occurs as a result of repetitive stress on the Achilles tendon. Over time, constant pressure on the already tight achilles tendon can damage the growth plate, causing children. Symptoms of Severs disease include pain and inflammation. This is why it is more common in physically active.
 Metatarsalgia is the name given to pain in the front part of your foot under the heads of your metatarsal bones ( ball of foot, just before toes). It is usually worse when standing or walking etc. and occurs most frequently in the second, third/or fourth metatarsal joints or isolated in the first metatarsal joint. Metatarsalgia usually comes on gradually over some weeks rather than suddenly. The affected area of your foot may also feel tender on palpation by your physiotherapist.
Metatarsalgia is the name given to pain in the front part of your foot under the heads of your metatarsal bones ( ball of foot, just before toes). It is usually worse when standing or walking etc. and occurs most frequently in the second, third/or fourth metatarsal joints or isolated in the first metatarsal joint. Metatarsalgia usually comes on gradually over some weeks rather than suddenly. The affected area of your foot may also feel tender on palpation by your physiotherapist. Plantar fasciitis is a painful inflammatory condition of the connective tissue on the sole of the foot(the plantar fascia). It is often caused by overuse of the plantar fascia, the tendons that help form the arch of the foot , running from the heel along the sole of the foot towards the toes. The plantar fascia
Plantar fasciitis is a painful inflammatory condition of the connective tissue on the sole of the foot(the plantar fascia). It is often caused by overuse of the plantar fascia, the tendons that help form the arch of the foot , running from the heel along the sole of the foot towards the toes. The plantar fascia