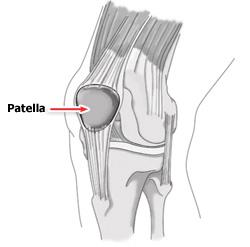
Patella Dislocation – knee Injury
The patella, or kneecap lies in front of the knee joint. It is attached to the quadriceps muscle via the quadriceps tendon and acts to increase the leverage from this muscle group when straightening the knee. The patella glides up and down virtically within a groove called the patello-femoral groove at the front of the thigh bone(femur) during knee bending. Patella dislocation occurs when the patella moves outside of this groove. The patella may also sublux rather than fully dislocate, meaning it only moves partially out of position. These injuries usually occurs as a result of an acute blow to or as a result of a twisting action on the knee. In most cases the patella will relocate into the patello-femoral groove on straightening of the knee. This, however is usually extremely painful. Risk factors which make a patella dislocation more likely are 1. insufficient quadriceps strength especially on the inside of the knee, 2. over pronation of the feet , and 3. an increased Q angle of the knee.
The vastus medialis obliqus muscle (VMO) is part of the quadriceps muscle group on the inside of the thigh, and is responsible for maintaining the stability of the patella towards the inside of the knee. If the VMO isn’t strong enough, the patella is much more susceptible to dislocation.
Over pronation of the feet is where the feet roll in(collapse in slightly on the flattened arch with the toes turning outwards) when running. This causes torsion at the knee, leaving the patella susceptible to moving outwards as the quadriceps contract.
The Q-angle of the knee is the angle formed by lines representing the pull of the quadriceps muscle and the axis of the patellar tendon. People with an increased Q ankle are often termed knock kneed. This angle when too large increases the risk of patellar dislocation.
Treatment of patella dislocation
Apply RICE(rest, ice, compression and elevation) principles to the injured knee . Ice can be applied for 10 to 15 minutes every hour initially reducing to 2 or 3 times a days as swelling and symptoms reduce. Also medications like non steroidal anti-inflammatories (NSAIDs), analgesics, pain killers etc. would be beneficial, in order to manage both the inflammation and the pain .
Rest from any sporting activities and seek medical advice. An athlete who has had one episode of patella dislocation is often susceptible to another. The knee may need to be immobilized for 2-3 weeks initially. A knee support can provide protection for the joint initially during rehab. Patella stabilizing braces have been specifically designed to provide support for the knee cap.
Quadriceps strengthening is initiated during this phase. These should be in the form of static exercises. Quadriceps electrical stimulation is an option for muscle reeducation if the patient has difficulty activating the muscle secondary to pain. Electrical stimulation may also play a role in the management of knee joint effusion. When swelling, inflammation has subsided, the patient may progress to the recovery phase of rehabilitation.
When the acute symptoms settle down a full knee strengthening rehabilitation program is required to help avoid future recurrence. Specifically exercises for the VMO muscle on the inside of the quadriceps are important, but overall quadriceps strengthening is also beneficial . The VMO is an important medial stabilizer of the patella. The prevailing theory has been that lateral patellar tracking is associated with VMO weakness. However, research has been inconclusive for VMO weakness as a direct causative mechanism of lateral patellar tracking(patellar subluxation/dislocation). Recent findings have shown that general quadriceps strengthening has demonstrated reductions in lateral tracking irrespective of the mechanism. Therapy should also include a protocol for hamstring muscle stretching. Tight hamstring muscles functionally counteract their agonist group, the quadriceps.
Any physical therapy program for patellofemoral problems must address any tightness or reduced flexibility in the quadriceps, hamstrings, hip abductors, iliotibial band and calf muscles.
Medial patellar gliding exercises may loosen lateral retinacular tightness in this stage. Medial patellar gliding exercises are performed with the leg extended. The patient manually pushes the patella medially and holds for a count of 10 seconds.
An important concept in the rehabilitation of patellar dislocation and patellofemoral pain is knee flexion. Initially, any activity that requires greater than 40-45° of knee flexion causes symptoms. Initial rehabilitation programs start with the isometric open kinetic chain . Early rehabilitation programs should limit all activities that require quadriceps firing with the knee flexed greater than 45°.
Once isometric open kinetic chain exercises are tolerated without discomfort, the rehabilitation program advances to closed kinetic chain exercises (eg, mini squats, lunges, stair climbing). The rectus femoris, VMO, and VL are all strengthened by the mini squats (repetitions and sets modified to the tolerance of the patient).
Important goals are to restore ”range of movement” in the joint, mobilize soft tissues, and strengthen the surrounding musculature. Lunges and bike riding allow strengthening through a controlled ”range of movement”. Once pain has resolved sufficiently to complete daily activity requirements without exacerbations, the patient can advance to the final phase of rehabilitation.
Advanced rehabilitation programs progress to jogging, running, plyometrics, and sport-specific exercises. Patients must be monitored and must always follow proper technique, as well as learn to properly fire the VMO.
Sometimes Surgery is needed. Most surgeons agree, if the kneecap dislocates multiple times, then surgery should be considered. When the kneecap dislocates, it is possible to damage the cartilage in the knee, leading to an increased risk of knee arthritis. When multiple dislocations occur, patellar stabilization surgery should be considered. While dislocations of the patella can occur after surgery, they are much less common.