When Back Pain Is A Symptom Rather Than A Condition
Back pain may sometimes be a symptom rather than a condition as such. A practitioner needs to always keep this at the back of their mind when treating or assessing somebody. Sometimes things need more investigation. A good physio will spot this early and refer you on quickly to your G.P. for further examination. It is always better to play it safe if in doubt. I always believe you should be seeing improvement in your condition from treatment to treatment. If there is no improvement after several treatments you need to be asking yourself a few questions i.e. Do I need to try a different physio or do I need to consult my doctor for a second opinion. Sometimes the proper treatment protocol for a condition is all that is needed for a swift recovery. The list below is not meant to be alarmist. It is more to emphasize the fact that continuous unrelenting back pain can be a symptom of something else going on within your body.
Below are examples of conditions/medications etc. that may have back pain as a side effect/symptom.
kidney stones – A kidney stone may not cause symptoms until it moves around within your kidney or passes into your ureter (the tube connecting the kidney and bladder). At that point, you may experience symptoms such as severe pain in your side and back below the ribs, or pain that radiates into the lower abdomen and groin.
Lupus is a long-term autoimmune disease in which the body’s immune system becomes hyperactive and attacks normal, healthy tissue. Symptoms include inflammation, swelling, and damage to the joints, skin, kidneys, blood, heart, and lungs. Lupus can cause neck and back pain, because muscles in these areas can become inflamed due to the lupus. Furthermore, the muscle pain syndrome ”fibromyalgia” can cause pain in these areas and is commonly associated with lupus.
Spinal arthritis/facet joint arthritis causes stiffness and back pain.
Cancers – A primary bone cancer tumor in the spine can cause back pain, as can a number of other cancers when they have metastasized(spread to other sites in the body), such as breast cancer, testicular cancer, colon cancer, and lung cancer. In fact, back pain is often the one of first symptoms that people with lung cancer notice before they are diagnosed. A tumor in the lungs can put pressure on the spine, or can affect the nerves around the chest wall and spine.
Spondylosis a painful condition of the spine resulting from the degeneration of the intervertebral discs.
Spondylitis is a condition resulting in inflammation within the joints of the spine. As the inflammation goes and healing takes place, bone grows out from both sides of the vertebrae and may join the two together, causing a stiffening known as ankylosis. The progressed condition is called ankylosing spondylitis. The cause is not yet known.
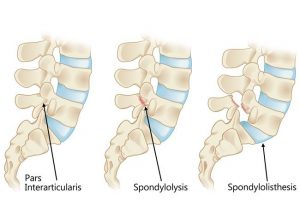
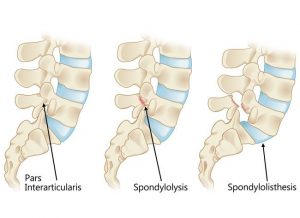
Spondylolisthesis is a slipping of vertebra that occurs, in most cases, at the base of the spine.
Spondylolysis is a defect or fracture of one or both wing-shaped parts of a vertebra, can result in vertebrae slipping backward, forward, or over a bone below.
Spondylosis, Spondylitis, Spondylolisthesis, Spondylolysis all have back pain as a symptom.
Fractures – Even a minor fracture along the spine can cause considerable back pain.
Statins – Statins are drugs that can help lower your cholesterol. One of the more severe side effect of statins is myotoxicity(having a toxic effect on muscle), in the form of myopathy(a disease of the muscle in which the muscle fibers do not function properly. This results in muscular weakness), myalgia(muscle pain), myositis(inflammation and degeneration of muscle tissue) or rhabdomyolysis(a condition in which damaged skeletal muscle breaks down). Currently, the only effective treatment of statin-induced myopathy is the discontinuation of statin use in patients affected by muscle aches, pains and elevated creatine kinase levels. Creatine kinase are the clinical measure of muscle damage (rhabdomyolysis).
Anticonvulsant drugs such those used in the treatment of conditions like epilepsy can cause changes in calcium and bone metabolism. This may in time lead to decreased bone mass and a risk of osteoporotic fractures in the spine which may also result in severe back pain. Two widely used antiepileptic drugs phenytoin and carbamazepine are recognized to have direct effects on bone cells.
For more about treatments and opening times etc. click on our homepage