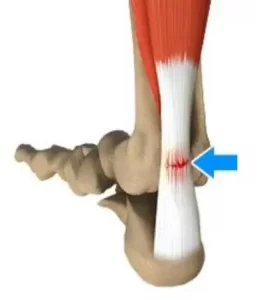
Achilles tendon ruptures will debilitate your lower leg completely, the moment they happen. The Achilles tendon is an important part of the leg. It is located just behind and above the heel, attaching the heel bone to the calf muscles. Its function is to help in bending the foot downwards at the ankle (this movement is called plantar flexion). If the Achilles tendon is torn/ruptured, the tear may be either partial or complete. In a partial tear, the tendon is torn but is still partly joined to the calf muscle. With complete tears, the tendon is completely torn and the connection between the calf muscles and the ankle bone is lost. If your Achilles tendon is ruptured you will be unable to stand on your tiptoes and you will have a flat-footed walk with a severe limp, along with considerable pain initially.
What causes Achilles tendon ruptures?
An Achilles tendon can tear when there is too high a load or stress placed on it. This can happen with activities involving a forceful push off with the foot – ie. running/sprinting in football, basketball, tennis etc. I have also seen it occur when somebody sprints off suddenly on a sandy beach, the sand giving way under the foot putting extra stress on the calf and the achilles tendon. The push off movement uses a strong contraction of the calf muscles maximally stressing both the calf muscles and the Achilles tendon . Injury to the achilles can also occur due to falls, if the foot is suddenly forced into an upward-pointing position, stretching the tendon. Another possible injury is a deep cut/laceration to the tendon.
Sometimes the Achilles tendon is weak, making it more prone to rupture. Factors that weaken the Achilles tendon are:
- Corticosteroid medications (such as prednisolone) – mainly when used as long-term treatment.
- A corticosteroid injection near the Achilles tendon.
- Certain rare medical conditions, such as Cushing’s syndrome, where the body makes too much of its own corticosteroid hormones.
- Tendinopathies of the Achilles tendon.
- Other medical conditions which can make the tendon more prone to rupture; for example, rheumatoid arthritis, diabetes, gout and systemic lupus erythematosus.
- Certain antibiotic medicines may slightly increase the risk of having an Achilles tendon rupture. These are the quinolone antibiotics such as ciprofloxacin and ofloacin. The risk of having an Achilles tendon rupture with these antibiotics is quite low and mainly applies to people who are also taking corticosteroid medication.
What are the symptoms of Achilles tendon ruptures?
You might hear a snap or feel a sudden sharp pain when the tendon is torn (ruptured)during a sporting activity or injury. The sharp pain usually settles quickly, although there may be some aching at the back of the lower leg. After the injury, the usual symptoms are:
- A flat-footed type of walk. You can walk and bear weight but cannot push off the ground properly on the side where the tendon is ruptured.
- Inability to stand on tiptoe.
- If the tendon is completely torn, you may feel a gap just above the back of the heel. However, if there is bruising and swelling may disguise the gap.
Diagnosis
An Achilles tendon rupture is usually diagnosed based on symptoms, history of the injury and a physio/doctor’s examination. An orthopedic test called Thompson’s test (also known as the calf squeeze test) may help diagnosis. In this test, you will be asked to lie face down on the examination bench and to bend your knee. The doctor will gently squeeze the calf muscles at the back of your leg and observe how the ankle moves. If the Achilles tendon is OK, the calf squeeze will make the foot point away from the leg (a movement called plantar flexion). This is quite an accurate test for Achilles tendon ruptures. An ultrasound or MRI may be used to confirm diagnosis and give a fuller picture of the injury.
Treatment and recovery
Treatment for a ruptured achilles tendon usually involves surgery to repair the tendon. The surgeon sews/sticks together the torn ends of the Achilles tendon, and may also use another tendon or a tendon graft to help with the repair. A plaster cast or brace is needed after the operation for about eight weeks, to keep the foot immobilized, allowing the tendon can heal. The plaster cast or the brace is positioned so that the foot is pointing slightly downwards, which takes the strain off the tendon.
Traditionally, crutches were used to keep weight off the leg during the first few weeks of treatment. Current thinking tends towards using the leg normally early on (early mobilization). This involves fitting a plaster cast or a brace which you can walk on. It is more convenient because you do not need to use crutches. Physiotherapy will also be needed, especially when the cast is removed. I have personally found instrument assisted soft tissue work(after about 8 weeks) to be very beneficial along with stretching/strengthening work and deep tissue work to the calf during recovery. Full recovery is greatly slowed when there is no hands-on work done during recovery, after the cast is removed once an ok is given by the surgeon to commence.
Depending on a person’s profession, some people may need several weeks off work after an Achilles tendon tear (rupture); the time taken to return to sport is usually between 4 and 12 months. Generally, the outlook is good. However, the tendon does take time to heal, usually about six to eight weeks. More time will be needed after this to allow the muscles and tendon to regain normal strength.
For more on rehabilitation on achilles tendon ruptures post surgery click here.
Physiotherapist in Tralee. Ring 08677001 to discuss your condition, book an appointment or get a second opinion.