When Back Pain Is A Symptom Rather Than A Condition
Back pain may sometimes be a symptom rather than a condition as such. A practitioner needs to always keep this at the back of their mind when treating or assessing somebody. Sometimes things need more investigation. A good physio will spot this early and refer you on quickly to your G.P. for further examination. It is always better to play it safe if in doubt. I always believe you should be seeing improvement in your condition from treatment to treatment. If there is no improvement after several treatments you need to be asking yourself a few questions i.e. Do I need to try a different physio or do I need to consult my doctor for a second opinion. Sometimes the proper treatment protocol for a condition is all that is needed for a swift recovery. The list below is not meant to be alarmist. It is more to emphasize the fact that continuous unrelenting back pain can be a symptom of something else going on within your body.
Below are examples of conditions/medications etc. that may have back pain as a side effect/symptom.
kidney stones – A kidney stone may not cause symptoms until it moves around within your kidney or passes into your ureter (the tube connecting the kidney and bladder). At that point, you may experience symptoms such as severe pain in your side and back below the ribs, or pain that radiates into the lower abdomen and groin.
Lupus is a long-term autoimmune disease in which the body’s immune system becomes hyperactive and attacks normal, healthy tissue. Symptoms include inflammation, swelling, and damage to the joints, skin, kidneys, blood, heart, and lungs. Lupus can cause neck and back pain, because muscles in these areas can become inflamed due to the lupus. Furthermore, the muscle pain syndrome ”fibromyalgia” can cause pain in these areas and is commonly associated with lupus.
Spinal arthritis/facet joint arthritis causes stiffness and back pain.
Cancers – A primary bone cancer tumor in the spine can cause back pain, as can a number of other cancers when they have metastasized(spread to other sites in the body), such as breast cancer, testicular cancer, colon cancer, and lung cancer. In fact, back pain is often the one of first symptoms that people with lung cancer notice before they are diagnosed. A tumor in the lungs can put pressure on the spine, or can affect the nerves around the chest wall and spine.
Spondylosis a painful condition of the spine resulting from the degeneration of the intervertebral discs.
Spondylitis is a condition resulting in inflammation within the joints of the spine. As the inflammation goes and healing takes place, bone grows out from both sides of the vertebrae and may join the two together, causing a stiffening known as ankylosis. The progressed condition is called ankylosing spondylitis. The cause is not yet known.
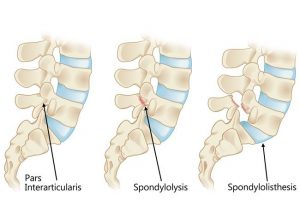
Spondylolisthesis is a slipping of vertebra that occurs, in most cases, at the base of the spine.
Spondylolysis is a defect or fracture of one or both wing-shaped parts of a vertebra, can result in vertebrae slipping backward, forward, or over a bone below.
Spondylosis, Spondylitis, Spondylolisthesis, Spondylolysis all have back pain as a symptom.
Fractures – Even a minor fracture along the spine can cause considerable back pain.
Statins – Statins are drugs that can help lower your cholesterol. One of the more severe side effect of statins is myotoxicity(having a toxic effect on muscle), in the form of myopathy(a disease of the muscle in which the muscle fibers do not function properly. This results in muscular weakness), myalgia(muscle pain), myositis(inflammation and degeneration of muscle tissue) or rhabdomyolysis(a condition in which damaged skeletal muscle breaks down). Currently, the only effective treatment of statin-induced myopathy is the discontinuation of statin use in patients affected by muscle aches, pains and elevated creatine kinase levels. Creatine kinase are the clinical measure of muscle damage (rhabdomyolysis).
Anticonvulsant drugs such those used in the treatment of conditions like epilepsy can cause changes in calcium and bone metabolism. This may in time lead to decreased bone mass and a risk of osteoporotic fractures in the spine which may also result in severe back pain. Two widely used antiepileptic drugs phenytoin and carbamazepine are recognized to have direct effects on bone cells.
For more about treatments and opening times etc. click on our homepage
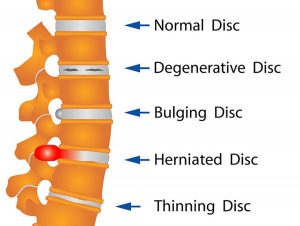 Your spine is made up of lots of bones called vertebrae and discs stacked on top of one another, forming the spinal canal. The nerves of the spinal cord run down the length of the spinal canal. The discs in act like shock absorbers between the vertebrae. These discs are made of two components: a softer center (called nucleus pulposus) surrounded by a tough elastic-like band (called annulus fibrosus). A bulging disc is like a squashed jam doughnut before the jam bursts out. The disc sags and looks like it is bulging outward. With a herniated disc, the outer covering of the disc has a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal. It is like the jam leaking out from the inside of a squashed jam doughnut.
Your spine is made up of lots of bones called vertebrae and discs stacked on top of one another, forming the spinal canal. The nerves of the spinal cord run down the length of the spinal canal. The discs in act like shock absorbers between the vertebrae. These discs are made of two components: a softer center (called nucleus pulposus) surrounded by a tough elastic-like band (called annulus fibrosus). A bulging disc is like a squashed jam doughnut before the jam bursts out. The disc sags and looks like it is bulging outward. With a herniated disc, the outer covering of the disc has a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal. It is like the jam leaking out from the inside of a squashed jam doughnut.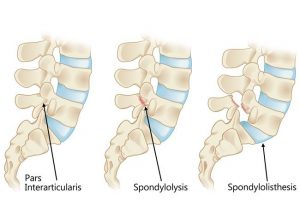
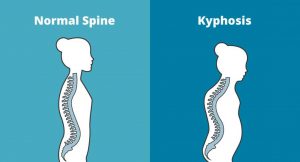 Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is more common in older people. Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time. Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfigurment. Treatment for kyphosis depends on your age, and both the cause and the effects of the curvature.
Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is more common in older people. Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time. Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfigurment. Treatment for kyphosis depends on your age, and both the cause and the effects of the curvature.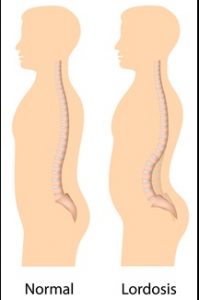 Some curvature in the lower back is normal. However, if your curve arches too far inward, it’s called lordosis, or swayback. Lordosis can affect your lower back and/or neck. The condition can lead to excess pressure on the spine, causing pain and discomfort. It can affect your ability to move if it’s severe and left untreated. Treatment of lordosis depends on how serious the curve is and how you got lordosis. There’s little medical concern if your lower back curve reverses itself when you bend forward. You can probably manage your condition with physical therapy and daily exercises.
Some curvature in the lower back is normal. However, if your curve arches too far inward, it’s called lordosis, or swayback. Lordosis can affect your lower back and/or neck. The condition can lead to excess pressure on the spine, causing pain and discomfort. It can affect your ability to move if it’s severe and left untreated. Treatment of lordosis depends on how serious the curve is and how you got lordosis. There’s little medical concern if your lower back curve reverses itself when you bend forward. You can probably manage your condition with physical therapy and daily exercises. Scoliosis is a medical condition in which a person’s spine curves sideways, usually in an “S” or “C” shape. In some, the degree of curvature remains stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, however severe cases can interfere with breathing. The cause of most cases is unknown, but is believed to involve a combination of genetic and environmental factors. Diagnosis is confirmed by Xray. Treatment depends on the degree of curve, location, and cause.
Scoliosis is a medical condition in which a person’s spine curves sideways, usually in an “S” or “C” shape. In some, the degree of curvature remains stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, however severe cases can interfere with breathing. The cause of most cases is unknown, but is believed to involve a combination of genetic and environmental factors. Diagnosis is confirmed by Xray. Treatment depends on the degree of curve, location, and cause. One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
