Everyone’s spine has curves, from your neck down to your lower back. These curves, which create the spine’s ”S” shape, are lordotic in shape in the neck and lower back, and kyphotic in shape for the upper back. They help your body 1. absorb shock, 2. support the weight of the head, 3. align your head over your pelvis, 4. stabilize and maintain its structure, 5. move and bend flexibly. When these curves are exaggerated through poor posture or hereditary conditions like scoliosis, spinal pain and problems can develop over time.
Kyphosis
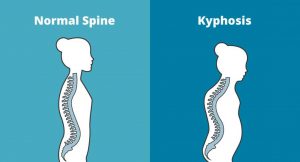 Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is more common in older people. Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time. Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfigurment. Treatment for kyphosis depends on your age, and both the cause and the effects of the curvature.
Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is more common in older people. Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time. Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfigurment. Treatment for kyphosis depends on your age, and both the cause and the effects of the curvature.
Lordosis
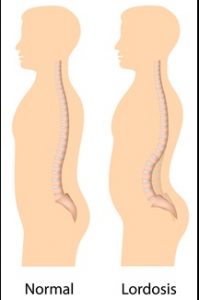 Some curvature in the lower back is normal. However, if your curve arches too far inward, it’s called lordosis, or swayback. Lordosis can affect your lower back and/or neck. The condition can lead to excess pressure on the spine, causing pain and discomfort. It can affect your ability to move if it’s severe and left untreated. Treatment of lordosis depends on how serious the curve is and how you got lordosis. There’s little medical concern if your lower back curve reverses itself when you bend forward. You can probably manage your condition with physical therapy and daily exercises.
Some curvature in the lower back is normal. However, if your curve arches too far inward, it’s called lordosis, or swayback. Lordosis can affect your lower back and/or neck. The condition can lead to excess pressure on the spine, causing pain and discomfort. It can affect your ability to move if it’s severe and left untreated. Treatment of lordosis depends on how serious the curve is and how you got lordosis. There’s little medical concern if your lower back curve reverses itself when you bend forward. You can probably manage your condition with physical therapy and daily exercises.
Scoliosis
 Scoliosis is a medical condition in which a person’s spine curves sideways, usually in an “S” or “C” shape. In some, the degree of curvature remains stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, however severe cases can interfere with breathing. The cause of most cases is unknown, but is believed to involve a combination of genetic and environmental factors. Diagnosis is confirmed by Xray. Treatment depends on the degree of curve, location, and cause.
Scoliosis is a medical condition in which a person’s spine curves sideways, usually in an “S” or “C” shape. In some, the degree of curvature remains stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, however severe cases can interfere with breathing. The cause of most cases is unknown, but is believed to involve a combination of genetic and environmental factors. Diagnosis is confirmed by Xray. Treatment depends on the degree of curve, location, and cause.
Minor curves may simply be watched periodically. Treatments may include bracing or surgery in more severe cases. The brace must be fitted to the person and used daily until growing stops. Evidence that chiropractic manipulation dietary supplements, or exercises can prevent the condition from worsening is non existent. However, exercise is still recommended due to its other health benefits. Scoliosis occurs in about 3% of people. It most commonly occurs between the ages of 10 and 20. Girls typically are more severely affected than boys.
Physiotherapists in Tralee Phone 086-7700191
 cartilage can be damaged by injury or normal wear and tear.
cartilage can be damaged by injury or normal wear and tear. Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.