Meniscus Injuries – Knee Pain
Meniscus injuries are a relatively common knee injury. Cartilage within the knee joint provides cushioning between the bones at this joint. This protects them from the stresses of walking, jumping, running etc. There is articular cartilage which is the smooth, white tissue that covers the ends of bones(Femur, tibia) where they come together to form the knee joint. Healthy cartilage in our joints makes it easier to move. It allows the bones to glide over each other with very little friction. Articular  cartilage can be damaged by injury or normal wear and tear.
cartilage can be damaged by injury or normal wear and tear.
Within the knee you also have fibrocartilage in the form of the medial and lateral meniscii. These are two thick wedge-shaped pads of cartilage attached to top of the tibia (tibial plateau) and under the femur bone. They allow the femur to glide when the knee joint moves. Each meniscus is curved in a C-shape, with the front part of the cartilage called the anterior horn and the back part called the posterior horn. Meniscal tears are usually described by where they are located anatomically in the C shape and by their appearance (for example, “bucket handle” tear, longitudinal, parrot beak, and transverse).
Blood supply
Because the blood supply is different to each part of the meniscus. Knowing where the tear is located may help decide how easily an injury might heal (with or without surgery). The better the blood supply, the better the potential for recovery. The outside rim of cartilage has better blood supply than the central part of the “C.” Blood supply to knee cartilage also decreases with age, with up to 20% of normal blood supply lost by age 40.
What causes a meniscus to tear?
A forceful twist or sudden stop can cause the end of the femur to grind into the top of the tibia, pinching and potentially tearing the cartilage of the meniscus. These meniscus injuries can also occur with deep squatting or kneeling, especially when lifting a heavy weight. Meniscus tear injuries often occur during athletic activities, especially in contact sports like football and hockey. Motions that require pivoting and sudden stops, in sports like tennis, basketball, and golf, can also cause meniscus damage.
Meniscus injuries – Increasing risk with age
The risk of developing a torn meniscus increases with age. This is because cartilage begins to gradually wear out, losing its blood supply and its resilience. Being overweight also puts more stress on the meniscii. This means that routine daily activities like walking and climbing stairs increase the potential for wear, degeneration, and tearing. It is estimated that six out of 10 patients older than 65 years have a degenerative meniscus tear. Many of these tears may never cause problems.
Some of the fibers of the cartilage are interconnected with those of the ligaments that surround the knee. Thus, meniscus injuries may also be associated with tears of the collateral and cruciate ligaments, depending upon the mechanism of injury.
Symptoms of meniscus injuries can include some or all of the following:
- Pain with running or walking longer distances
- Intermittent swelling of the knee joint: Many times, the knee with a torn meniscus feels “tight.”
- Popping, especially when climbing up or down stairs
- Giving way or buckling (the sensation that the knee is unstable and the feeling that the knee will give way): Less commonly, the knee actually will give way and cause the patient to fall.
- Locking (a mechanical block where the knee cannot be fully extended or straightened): This occurs when a piece of torn meniscus folds on itself and blocks full range of motion of the knee joint. The knee gets “stuck,” usually flexed between 15 and 30 degrees and cannot bend or straighten from that position.
Diagnosis
The diagnosis of a knee injury begins with a history of the injury etc. and physical examination. There have been many tests described to assess the internal structures of the knee. The McMurray test is one long used orthopedic test . The health-care professional flexes the knee and rotates the tibia while feeling along the joint. The test is positive for a potential tear if a click is felt or noticeable pain is felt while circumducting the knee in full flexion.
Physiotherapy in Tralee – referral for MRI
(MRI) is the test of choice to confirm the diagnosis of a torn meniscus. It also allows a radiographer to visualize the inner structures of the knee. These structure include; the cartilage and ligaments, the surface of the bones, and the muscles and tendons that surround the knee joint. Plain X-rays cannot be used to identify meniscal tears but may be helpful in looking for bony changes, including fractures, arthritis, and loose bony fragments within the joint. In older patients, X-rays may be taken of both knees while the patient is standing. This allows the joint spaces to be compared to assess the degree of cartilage wear. Cartilage takes up space within the joint and if the joint space is narrowed, it may be an indicator that there is less cartilage present, likely from degenerative disease.
Treatment of Meniscal Tears
Sometimes conservative measures such as physical therapy, NSAIDs and rest can be enough to settle the condition. When conservative measures are ineffective the next step may be surgery to repair or remove the damaged cartilage.
Here is a little video explaining more.
For physiotherapy in Tralee phone 086-7700191, click here for website homepage

 cartilage can be damaged by injury or normal wear and tear.
cartilage can be damaged by injury or normal wear and tear. Dry Needling
Dry Needling
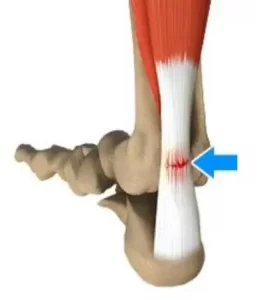
 Posterior ankle impingement is a condition characterised by tissue damage at the back of
Posterior ankle impingement is a condition characterised by tissue damage at the back of
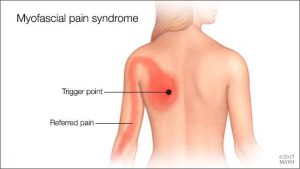 Myofascial Pain Syndrome
Myofascial Pain Syndrome Instrument Assisted Soft Tissue Mobilization, also known as ”IASTM” for short is a process in which the clinician uses a set of ergonomically designed hand held instruments to break down the scar tissue and fascial restrictions in soft tissue (muscles, ligaments, tendons, and fascia ). The instruments you see in the photo are made of surgical grade stainless steel. Hypoallergenic aqueous cream or massage oil is used to facilitate gliding of the instrument along the muscle, tendon etc. during treatment. The technique itself is said to have evolved from a form of Traditional Chinese Medicine called Gua Sha. IASTM is a is a procedure that is growing rapidly in popularity due to both the effectiveness and efficiency 0f the technique.
Instrument Assisted Soft Tissue Mobilization, also known as ”IASTM” for short is a process in which the clinician uses a set of ergonomically designed hand held instruments to break down the scar tissue and fascial restrictions in soft tissue (muscles, ligaments, tendons, and fascia ). The instruments you see in the photo are made of surgical grade stainless steel. Hypoallergenic aqueous cream or massage oil is used to facilitate gliding of the instrument along the muscle, tendon etc. during treatment. The technique itself is said to have evolved from a form of Traditional Chinese Medicine called Gua Sha. IASTM is a is a procedure that is growing rapidly in popularity due to both the effectiveness and efficiency 0f the technique.