Chondromalacia Patella – Knee Pain – Patellar Tracking Dysfunction
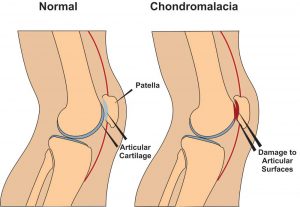 Chondromalacia patella, also known as ”Runners Knee” is one of the most common causes of knee pain in runners. The condition results from irritation of the cartilage on the under-surface of the kneecap. This cartilage is smooth and the kneecap normally glides effortlessly across it during bending of the knee joint. In some individuals however the kneecap does not track so smoothly due to poor alignment and the cartilage surface becomes irritated, resulting in inflammation and knee pain. In more severe cases there can be breakdown of the cartilage. Chondromalacia patella can affect athletes of any age but tends to be more common in women, most likely due to anatomical differences between the sexes ie. wider hips in females which results in a greater angulation between hip and knee, thus resulting in increased lateral forces on the patella.
Chondromalacia patella, also known as ”Runners Knee” is one of the most common causes of knee pain in runners. The condition results from irritation of the cartilage on the under-surface of the kneecap. This cartilage is smooth and the kneecap normally glides effortlessly across it during bending of the knee joint. In some individuals however the kneecap does not track so smoothly due to poor alignment and the cartilage surface becomes irritated, resulting in inflammation and knee pain. In more severe cases there can be breakdown of the cartilage. Chondromalacia patella can affect athletes of any age but tends to be more common in women, most likely due to anatomical differences between the sexes ie. wider hips in females which results in a greater angulation between hip and knee, thus resulting in increased lateral forces on the patella.
Chondromalacia Patella – Causes
There are several causes both structural and dynamic which are linked to the condition. These include excessive foot pronation(feet turn out when running etc.), tight IT band, tight vastus lateralis(basically outer lower quad), weak or slow firing vastus medialis (basically lower inner quad), increased Q angle (simply put the angle between the outer hip and centre of the knee), a lateral femoral condyle that is not sufficiently prominent anteriorly (simply put the knee joint does not fit together properly),and a small or high riding patella(knee cap).(McConnell, 2002)
Chondromalacia Patella – Symptoms
The most common symptom is a dull, aching pain in the front of the knee, behind the kneecap. This pain is often worse when you go up or down stairs. It also can flare up after you have been sitting in one position for a long time. For example, your knee may be painful and stiff when you stand up after watching a movie or after a long trip in a car or plane. In some cases, the painful knee also can appear puffy or swollen. Chondromalacia can sometimes cause a creaky sound or grinding sensation known as ”crepitus” when you move your knee.
Chondromalacia Patella – Physio Treatment
Suitable treatment may involve 1. Soft tissue work to loosen tightened structures such as vastus lateralis muscle, IT band, lateral retinaculum etc., 2.Strengthening of weak structures such as vastus medialis, glutes , hip abductors etc., 3. Correction of overpronation using orthotics, 4. Non steroidal anti-inflammatories such as ibuprofen to reduce pain and inflammation, 5. Rest with gradual return to exercise, 6. Taping to correct tracking can be a short term solution.(Hertling and Kessler, 2006) while you strengthen the vastus medialis muscle. Also there are supports you can purchase to help correct patella tracking while exercising. These are a good short term solution while you correct the problems referred to above. Here is a good example.
If nonsurgical treatments fail, or if you have severe symptoms, your doctor may recommend arthroscopy to check the cartilage inside your knee. If the cartilage is softened or shredded, damaged layers can be removed during the surgery, leaving healthy cartilage in place .
References
Hertling, D., Kessler, R.M. ”Management of Common Musculoskeletal Disorders : Physical Therapy Principles and Methods.” Lippincott, Philidelphia 524-533, 2006.
Mc Connell, J. ”The physical therapist’s approach to patellofemoral disorders.” Clinical Sports Medicine 21:363-387, 2002.
For more information on chondromalacia patella see this video.
If you would like to get in touch to discuss your condition or make an appointment for physio in Tralee, please click
here for details.
Regards Eddie.
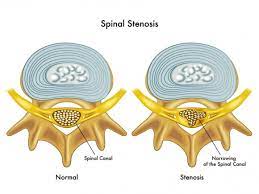 Spinal stenosis is a narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. Others may experience pain, tingling, numbness and muscle weakness. Symptoms often start gradually and worsen over time. Spinal stenosis is most commonly caused by wear-and-tear changes in the spine related to osteoarthritis. In severe cases of spinal stenosis, doctors may recommend surgery to create additional space for the spinal cord or nerves. Most people with spinal stenosis are over the age of 50. There are two main types of spinal stenosis: 1. Cervical stenosis. where the narrowing occurs in your neck. 2. Lumbar stenosis where the narrowing occurs in the lower back.
Spinal stenosis is a narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. Others may experience pain, tingling, numbness and muscle weakness. Symptoms often start gradually and worsen over time. Spinal stenosis is most commonly caused by wear-and-tear changes in the spine related to osteoarthritis. In severe cases of spinal stenosis, doctors may recommend surgery to create additional space for the spinal cord or nerves. Most people with spinal stenosis are over the age of 50. There are two main types of spinal stenosis: 1. Cervical stenosis. where the narrowing occurs in your neck. 2. Lumbar stenosis where the narrowing occurs in the lower back.