What is Hallux Rigidus?
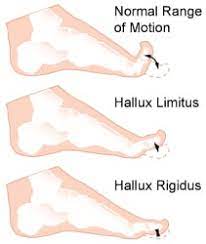
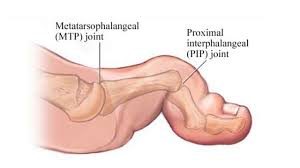
Big toe joint arthritis (otherwise known as Hallux Rigidus) is a form of degenerative arthritis. In this condition, surfaces of the joints in the big toe begin to wear away and extra bone can also develop in the form of bone spurs or osteophytes. This limits the movement of the joint. The big toe needs to bend significantly when stepping off. Consequently, arthritis in this joint can greatly affect walking, running etc.
Hallux Rigidus is a condition that tends to get worse over time. In it’s earlier stages, it may be referred to as Hallux Limitus, which is where there is limited movement of the big toe joint. With progression, Hallux Rigidus develops which can result in stiffness developing in the big toe joint and there may also be swelling.
To compensate for pain in the big toe joint, people with Hallux Rigidus tend to adjust their walking pattern which can also result in knee, hip or lower back pain. There is often difficulty finding shoes that fit properly shoes due to pain and/or inflammation in the joint. Early diagnosis can be made by physical examination and x-ray. Early treatment gives the best chance of avoiding surgery.
What causes Hallux Rigidus?
The big toe joint is designed to bear a considerable amount of stress during walking. However faulty biomechanics or structural abnormalities such as flat feet can stop the big toe from bending normally, and eventually lead to the development of osteoarthritis in the big toe joint. Other factors that can increase the risk of developing this condition include genetics (eg, having a certain foot type), injury to the big toe , other inflammatory diseases, and working in a job that places excessive stress on the big toe joint .
Treatment
In cases of Hallux Rigidus, certain types of footwear and orthotics may be recommended to reduce pressure and motion on the big toe. Custom orthotics that conform very closely to the arch of the foot are most effective in improving big toe joint function. These orthotics may incorporate something like a 3mm kinetic wedge in combination with a built in forefoot posting to take the pressure off the big toe joint. Ice and anti-inflammatory medication can also be used to reduce inflammation and pain. If it does not respond to conservative treatment, surgery may be recommended as a last resort in more severe cases.
 Posterior ankle impingement is a condition characterised by tissue damage at the back of
Posterior ankle impingement is a condition characterised by tissue damage at the back of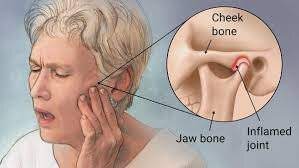 The temporomandibular joint works as a combination of hinge and sliding actions. It connects the jawbone to the skull on each side of the face. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth. Temporomandibular joint disorder (TMJD) can cause pain in your jaw joint and in the muscles that control jaw movement.
The temporomandibular joint works as a combination of hinge and sliding actions. It connects the jawbone to the skull on each side of the face. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth. Temporomandibular joint disorder (TMJD) can cause pain in your jaw joint and in the muscles that control jaw movement.
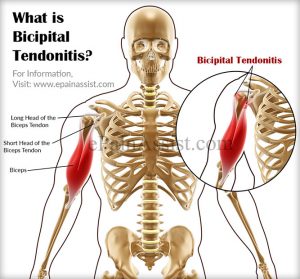 Bicipital tendonitis is a common cause of shoulder pain, often developing in people who perform repetitive, overhead movements. Biceps tendinitis develops over time, the pain being located at the front of the shoulder. The biceps muscle has two parts referred to as the long head and the short head. The tendon of the long head of the biceps is most commonly implicated with tendonitis. When this tendon is subjected to repetitive stresses, it can become irritated, swollen, and painful.This occurs where the tendon sits within the bicipital groove at the top of the humerus under the transverse ligament before it becomes part of the shoulder joint capsule.
Bicipital tendonitis is a common cause of shoulder pain, often developing in people who perform repetitive, overhead movements. Biceps tendinitis develops over time, the pain being located at the front of the shoulder. The biceps muscle has two parts referred to as the long head and the short head. The tendon of the long head of the biceps is most commonly implicated with tendonitis. When this tendon is subjected to repetitive stresses, it can become irritated, swollen, and painful.This occurs where the tendon sits within the bicipital groove at the top of the humerus under the transverse ligament before it becomes part of the shoulder joint capsule.
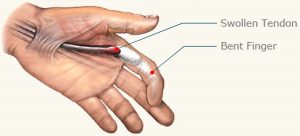 Trigger finger is a condition in which one of your fingers gets stuck in a bent position. Your finger may bend or straighten with a snap — like a trigger being pulled and released.
Trigger finger is a condition in which one of your fingers gets stuck in a bent position. Your finger may bend or straighten with a snap — like a trigger being pulled and released. Instrument Assisted Soft Tissue Mobilization, also known as ”IASTM” for short is a process in which the clinician uses a set of ergonomically designed hand held instruments to break down the scar tissue and fascial restrictions in soft tissue (muscles, ligaments, tendons, and fascia ). The instruments you see in the photo are made of surgical grade stainless steel. Hypoallergenic aqueous cream or massage oil is used to facilitate gliding of the instrument along the muscle, tendon etc. during treatment. The technique itself is said to have evolved from a form of Traditional Chinese Medicine called Gua Sha. IASTM is a is a procedure that is growing rapidly in popularity due to both the effectiveness and efficiency 0f the technique.
Instrument Assisted Soft Tissue Mobilization, also known as ”IASTM” for short is a process in which the clinician uses a set of ergonomically designed hand held instruments to break down the scar tissue and fascial restrictions in soft tissue (muscles, ligaments, tendons, and fascia ). The instruments you see in the photo are made of surgical grade stainless steel. Hypoallergenic aqueous cream or massage oil is used to facilitate gliding of the instrument along the muscle, tendon etc. during treatment. The technique itself is said to have evolved from a form of Traditional Chinese Medicine called Gua Sha. IASTM is a is a procedure that is growing rapidly in popularity due to both the effectiveness and efficiency 0f the technique.

