Snapping Hip – Physiotherapist Tralee
Snapping hip syndrome is a clinical condition characterized by a palpable or audible snapping sensation in the hip area when walking, climbing a stairs, squatting or swinging your leg around etc. Although the condition is usually painless and harmless, the sensation can be annoying. In some cases, snapping hip leads to a bursitis, a painful swelling of the fluid-filled sacs that cushion tendons from bones of the hip joint, during movement. Snapping hip can also occur in other areas of the hip where tendons and muscles slide over knobbly areas on the hip bones. These areas include :
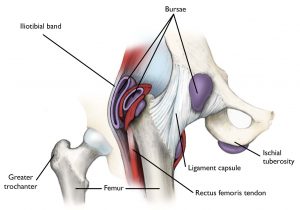
- Outside of the hip : This is the most common, where the iliotibial band passes over the portion of the thighbone known as the greater trochanter. When the hip is straight, the iliotibial band is behind the trochanter. When the hip bends, the band moves over the trochanter so that it is in front of it. The iliotibial band is always tight, like a stretched rubber band. Because the trochanter juts out slightly, the movement of the band across it creates the snap you hear. Eventually, snapping hip may lead to hip bursitis.
- Front of the hip. Another tendon at the front of the hip that could cause snapping hip runs from the front of the thigh up to the pelvis is the rectus femoris tendon. As you bend the hip, the tendon shifts across the head of the thighbone, and when you straighten the hip, the tendon moves back to the side of the thighbone. This back-and-forth motion across the head of the thighbone causes the snapping. The iliopsoas tendon can also catch on bony prominences at the front of the pelvis bone.
- Back of the hip. Snapping in the back of the hip can involve the hamstring tendon. This tendon attaches to the sitting bone, called the ischial tuberosity. When it moves across the ischial tuberosity, the tendon may catch, causing a snapping sensation in the buttock region. This is rare.
Cause of snapping hip
It is most often the result of tightness in the muscles and tendons surrounding the hip. Athletes in sports that require repetitive hip flexing are more likely to experience snapping hip. Young athletes can also be prone because tightness in the muscle structures of the hip due to adolescent growth spurts.
Treatment
Stretching the muscles of the affected areas ie. stretching of piriformis, tensor fascia latae, psoas/iliopsoas muscle, rectus femoris. Sometimes strengthening of the hip area may also be required to balance out the area, but usually the condition is a result of tight muscles and/or overuse, so stretching and rest, or activity modification is most effective.
In the rare instances that snapping hip does not respond to conservative treatment, your doctor may recommend surgery. The type of surgery will depend on the cause of the snapping hip. A bursitis can be cut out with surgery or often a cortisone injection is enough to settle it down.
Interesting articles on the condition include:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4961351/
https://link.springer.com/article/10.1007/s00167-020-06305-w
For more information phone us and talk to one of our physiotherapists in Tralee, or click here.
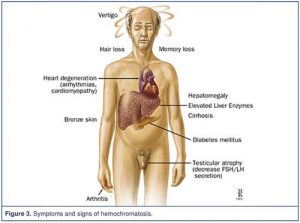 Haemochromatosis is a inherited condition where iron levels in the body increase over many years leading to iron overload. If the condition is not treated, it can lead to damage in certain parts of the
Haemochromatosis is a inherited condition where iron levels in the body increase over many years leading to iron overload. If the condition is not treated, it can lead to damage in certain parts of the