
Equinus Foot Condition
The ankle joint connects the leg to the foot. It is formed by three separate bones, the tibia, fibula and talus. The shinbone (tibia) supports most of a person’s weight when standing. The outer bone (fibula) is the smaller bone of the lower leg. A small, irregular-shaped foot bone (talus) connects the tibia and fibula. Acting as a hinge, these bones form the ankle. The ankle joint allows movement such as walking, running and jumping, and also contributes to lower limb stability.
The ankle is reinforced by ligaments which connect bone to bone. Ligaments have a mildly elastic structure that allows them to stretch, within their limits, and then return to their normal positions. Ligaments protect the ankle from abnormal movements—especially twisting, turning and rolling of the foot.
Description
A person with equinus has a limited range of ankle motion and lacks the flexibility needed to bring the top of the foot upward, toward the shin. It may be either congenital or acquired, and occurs equally in both men and women. Equinus can be due to several different reasons including the following:
• bony block between the talus and distal tibia (osseous equinus);
• contracture or tightness of the soleus muscle (inner calf muscle);
• contracture or tightness of the soleus and gastrocnemius muscles (gastroc-soleal equinus);
• isolated tightness of the gastrocnemius muscles (outer calf muscle); and
• compensatory loss of ankle joint range of motion for some other condition such as pes cavus (pseudoequinus).
People with equinus often develop ways to compensate for their limited ankle motion. Depending on how a patient compensates for the inability to bend properly at the ankle, a variety of other foot conditions can develop, such as:
- Plantar Fasciitis
- Calf cramping
- Achilles Tendinitis
- Metatarsalgia (pain and/or callusing on the ball of the foot)
- Flatfoot
- Arthritis of the midfoot (middle area of the foot)
- Pressure sores on the ball of the foot or the arch
- Bunions and hammertoes
- Ankle pain
- Shin splints
- Sesamoiditis
- Hallux valgus
- hallux rigidus
- Hammer toes
Nonsurgical Treatment of Equinus
Some nonsurgical treatment strategies are aimed at relieving the symptoms and conditions associated with equinus. Treatment for the equinus itself may include one or more of the following options.
- Heel lifts—Placing heel lifts inside the shoes or wearing shoes with a moderate heel may reduce symptoms by taking stress off the Achilles tendon and compensating for the restricted movement of the ankle joint. The joint is meant to have about fourteen degrees of movement ideally, so say it has only four degrees of movement, adding a ten degree heel lift helps compensate for the missing degrees of movement .
- Arch supports or orthotic devices—Custom orthotic devices that fit into the shoe are often prescribed to ensure that weight is distributed properly, and to help control muscle/tendon imbalance. Again these devices will most likely include a heel lift.
- Physical therapy—To help remedy muscle tightness, deep tissue massage of calf muscles along with a stretching program for the calf muscles are recommended.
For a quick simple video describing the condition click here
See our wide range of orthotics here
 Posterior ankle impingement is a condition characterised by tissue damage at the back of
Posterior ankle impingement is a condition characterised by tissue damage at the back of
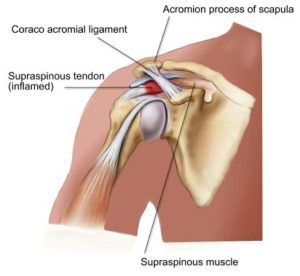 Shoulder impingement is a very common cause of shoulder pain, where a supraspinatus tendon inside the shoulder rubs or catches on nearby tissue and/or bone(acromium) as you lift your arm.
Shoulder impingement is a very common cause of shoulder pain, where a supraspinatus tendon inside the shoulder rubs or catches on nearby tissue and/or bone(acromium) as you lift your arm. 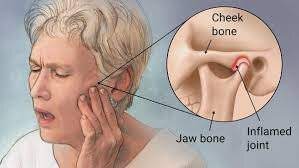 The temporomandibular joint works as a combination of hinge and sliding actions. It connects the jawbone to the skull on each side of the face. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth. Temporomandibular joint disorder (TMJD) can cause pain in your jaw joint and in the muscles that control jaw movement.
The temporomandibular joint works as a combination of hinge and sliding actions. It connects the jawbone to the skull on each side of the face. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth. Temporomandibular joint disorder (TMJD) can cause pain in your jaw joint and in the muscles that control jaw movement.
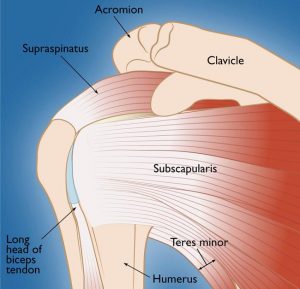 Rotator Cuff Tears
Rotator Cuff Tears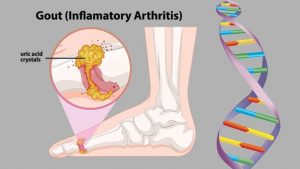 Gout is a form of arthritis which starts as a result of excess uric acid build-up in the blood, also called hyperuricemia. It is an extremely painful condition. Uric acid is produced in the body during the breakdown of purines – chemical compounds that are found in certain foods such as meat, poultry, and seafood. Normally, uric acid is dissolved in the blood and is excreted from the body in the urine via the kidneys. If too much uric acid is produced, it can build up and form needle-like crystals that trigger inflammation and pain in the joints and surrounding tissue. The condition often starts by affecting the joint at the base of the big toe. Attacks often occur without warning and in the middle of the night. They can come on quickly and keep returning over time, slowly damaging tissues in the region of the inflammation.
Gout is a form of arthritis which starts as a result of excess uric acid build-up in the blood, also called hyperuricemia. It is an extremely painful condition. Uric acid is produced in the body during the breakdown of purines – chemical compounds that are found in certain foods such as meat, poultry, and seafood. Normally, uric acid is dissolved in the blood and is excreted from the body in the urine via the kidneys. If too much uric acid is produced, it can build up and form needle-like crystals that trigger inflammation and pain in the joints and surrounding tissue. The condition often starts by affecting the joint at the base of the big toe. Attacks often occur without warning and in the middle of the night. They can come on quickly and keep returning over time, slowly damaging tissues in the region of the inflammation. Spinal stenosis is a narrowing of the space within the spine. This can put pressure on the nerves that travel through the spine. It occurs most often in the lower back and the neck. Some people are born with a congenital form, but most develop it as part of the degenerative cascade. Sometimes people do not feel effects of the narrowing, but as part of the aging process, most people will eventually notice radiating pain, weakness, and/or numbness secondary to the compression of the nerves or spinal cord. In lumbar stenosis, the spinal nerve roots in the lower back become compressed and this can produce – tingling, weakness or numbness that radiates from the low back and into the buttocks and legs, especially with activity.
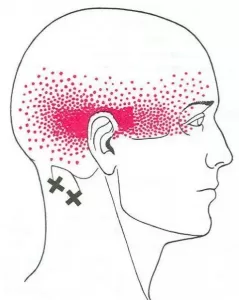
Spinal stenosis is a narrowing of the space within the spine. This can put pressure on the nerves that travel through the spine. It occurs most often in the lower back and the neck. Some people are born with a congenital form, but most develop it as part of the degenerative cascade. Sometimes people do not feel effects of the narrowing, but as part of the aging process, most people will eventually notice radiating pain, weakness, and/or numbness secondary to the compression of the nerves or spinal cord. In lumbar stenosis, the spinal nerve roots in the lower back become compressed and this can produce – tingling, weakness or numbness that radiates from the low back and into the buttocks and legs, especially with activity.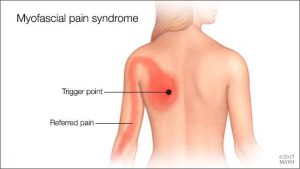 Myofascial Pain Syndrome
Myofascial Pain Syndrome