Tennis Elbow Misdiagnosis
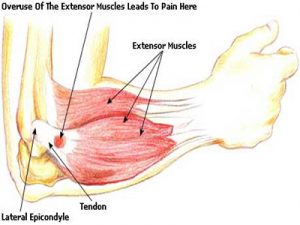
Tennis elbow, or lateral epicondylitis, is a painful condition of the elbow usually caused by overuse. Muscles, ligaments, and tendons support the functioning of the elbow joint. Your forearm extensor muscles and tendons extend the wrist and fingers. These extensor tendons attach the forearm muscles on the outside of the elbow to the lateral epicondyle. Tennis elbow is an injury to these tendons leading to pain and tenderness on the outside of the elbow. The main tendon involved in tennis elbow is usually the ”extensor carpi radialis brevis” tendon . Tennis elbow misdiagnosis is relatively common.
Tennis Elbow
When the tendon is weakened from overuse or trauma , microscopic tears form in the where the tendon attaches to the lateral epicondyle. This leads to pain and inflammation. The extensor carpi radialis brevis tendon may also be at increased risk of damage due to its position. As the elbow bends and straightens, the tendon rubs against the bone. This repetitive action can cause gradual wear and tear on the tendon over time in certain activities.
Activities – cause
Athletes are not the only people who get tennis elbow. Many people with tennis elbow participate in work or recreational activities that require repetitive and vigorous use of the forearm muscle. Painters, plumbers, carpenters, hairdressers, barbers, butchers(boners), people cutting hedges with clippers for long periods, are all particularly prone to developing tennis elbow.
Misdiagnosis
Tennis elbow misdiagnosis and mismanagement of this condition is often why people fail to recover. There are two common areas of misdiagnosis. Firstly if a person has not been doing any repetitive work with their forearm and there has been no forceful trauma while using the forearm, it is unlikely that the condition is tennis elbow. Sometimes the actual issue here is nerve pain radiating down the arm from nerve compression in the neck and/or shoulder(neuropraxia). This nerve compression can be due to tight muscles/ locked facet joints and/or misaligned structures, often due to poor posture. In the second type of tennis elbow misdiagnosis there can be repetitive injury involved but the condition is being exacerbated by nerve compression in the neck and shoulders, so both all areas need to be looked at for full resolution.
A cortisone injection is often used to try and treat ”tennis elbow”. This at most usually only gives short term relief and can even exacerbate the condition long-term with true tennis elbow, as it often allows the person to return to the aggravating activity thinking the injury has healed. Cortisone is an anti-inflammatory and may decrease inflammation in the area, reducing pain. It does not however stimulate tendon repair, which is what has been damaged in true ”tennis elbow” . Neither does cortisone do anything for a trapped nerve.
The above conditions are where an experienced physiotherapist/physical therapist can help greatly, usually much more so than any medication. This is their area of expertise. However, you always need to remember accurate diagnosis and effective treatment is very practitioner dependent. Eccentric training along with soft tissue work can be very effective for true ”tennis elbow”. For the nerve compression (neuropraxia) described above, soft tissue release of neck and shoulder muscles(levator scapulae, trapezius,scalenes etc.) along with osteopathic manipulations to release any locked cervical or thoracic facet joints can be very effective. Symptoms of nerve entrapment/involvement can include neck/shoulder pain with tingling down the arms and/or into fingers. There are also manual orthopedic tests to check for nerve entrapment.
Aside : Carpal Tunnel syndrome is a medical condition due to compression of the median nerve as it travels through the wrist at the carpal tunnel. This can also be misdiagnosed and be due to nerve compression in neck /shoulder or upper thoracic regions.
Physiotherapists in Tralee phone 086-7700191
 Muscles are made up of fibers that your nerves control. Muscle twitching is caused by minor muscle contraction in the area, or uncontrollable twitching of a muscle group that is served by a single motor nerve fiber. Stimulation or damage to a nerve may cause your muscle fibers to twitch. Most muscle twitches are minor and aren’t usually a cause for concern. Some are common and normal. Others are signs of a nervous system disorder.
Muscles are made up of fibers that your nerves control. Muscle twitching is caused by minor muscle contraction in the area, or uncontrollable twitching of a muscle group that is served by a single motor nerve fiber. Stimulation or damage to a nerve may cause your muscle fibers to twitch. Most muscle twitches are minor and aren’t usually a cause for concern. Some are common and normal. Others are signs of a nervous system disorder.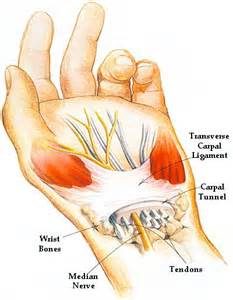 Carpal tunnel syndrome is a condition that causes numbness, tingling and weakness in the hand and arm. The condition is caused by compression of the median nerve within the carpal tunnel, a narrow passageway on the palm side of your wrist. The median nerve runs from your neck down along the arm and through the carpal tunnel to your hand. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb . Anything that squeezes or irritates the median nerve in the carpal tunnel space may lead to this condition. The anatomy of your wrist, health problems and possibly repetitive hand motions may also contribute. A wrist fracture can narrow the carpal tunnel and irritate the nerve, as can the swelling and inflammation resulting from rheumatoid arthritis.
Carpal tunnel syndrome is a condition that causes numbness, tingling and weakness in the hand and arm. The condition is caused by compression of the median nerve within the carpal tunnel, a narrow passageway on the palm side of your wrist. The median nerve runs from your neck down along the arm and through the carpal tunnel to your hand. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb . Anything that squeezes or irritates the median nerve in the carpal tunnel space may lead to this condition. The anatomy of your wrist, health problems and possibly repetitive hand motions may also contribute. A wrist fracture can narrow the carpal tunnel and irritate the nerve, as can the swelling and inflammation resulting from rheumatoid arthritis. Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
Restless legs syndrome(RLS) is a nervous system disorder resulting in an urge to move the legs. Because it usually interferes with sleep, it also is considered a sleep disorder. The condition causes an uncomfortable, “itchy,” “pins and needles,” or “creepy crawly” type feeling in the legs. These sensations are usually worse at rest, especially when lying or sitting. The symptoms are generally also worse in the evening and at night. The severity of RLS symptoms varies from mild to intolerable. Symptoms can come and go and vary widely in severity. For some people, symptoms may lead to severe sleep disturbance at night. This can significantly impair their quality of life.
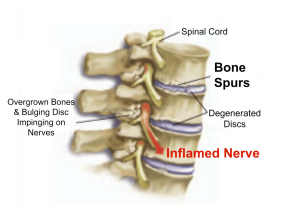 Bone spurs may or may not cause symptoms. Symptoms are location dependent. If bone spurs rub against other bones at joints they can cause pain and/or more limited movement in these joints. They can also be associated with pain, numbness, tenderness, and /or weakness in areas where they irritate adjacent tissue structures(muscles, ligaments, bones, nerves etc.). If the bone spur rubs against tendons or ligaments, they can sometimes cause a tear in these tissues over time. This is a common cause of tears in certain rotator cuff tendons .
Bone spurs may or may not cause symptoms. Symptoms are location dependent. If bone spurs rub against other bones at joints they can cause pain and/or more limited movement in these joints. They can also be associated with pain, numbness, tenderness, and /or weakness in areas where they irritate adjacent tissue structures(muscles, ligaments, bones, nerves etc.). If the bone spur rubs against tendons or ligaments, they can sometimes cause a tear in these tissues over time. This is a common cause of tears in certain rotator cuff tendons . A ”dead leg”, also known as ”charley horse” or ”quadriceps contusion”, is essentially an injury due to a traumatic blow, crushing the quadriceps muscle against the femur bone. The quadriceps is the muscle at the front of your thigh. The injury can be either intermuscular or intramuscular. Treatment depends on the type of contusion and grade in severity of the injury. An Intramuscular contusion occurs when the muscle gets torn within the sheath surrounding it. This causes the initial bleeding to cease within hours due to increased pressure within the muscle. However, the fluid and blood is not able to escape from the muscle sheath surrounding it resulting in considerable loss of function and a lot of pain. This can take days or weeks for a full recovery. You are unlikely to see any bruising with this type of contusion, especially in the early stages. In the case of intermuscular contusions, the muscle as well as part of the sheath surrounding it gets torn. This results in a longer bleeding time initially, especially if there is no use of ice therapy. The patient usually recovers faster from this type of dead leg, as the blood and fluids can easily flow away from the injury site. Bruising is often present in this type of contusion.
A ”dead leg”, also known as ”charley horse” or ”quadriceps contusion”, is essentially an injury due to a traumatic blow, crushing the quadriceps muscle against the femur bone. The quadriceps is the muscle at the front of your thigh. The injury can be either intermuscular or intramuscular. Treatment depends on the type of contusion and grade in severity of the injury. An Intramuscular contusion occurs when the muscle gets torn within the sheath surrounding it. This causes the initial bleeding to cease within hours due to increased pressure within the muscle. However, the fluid and blood is not able to escape from the muscle sheath surrounding it resulting in considerable loss of function and a lot of pain. This can take days or weeks for a full recovery. You are unlikely to see any bruising with this type of contusion, especially in the early stages. In the case of intermuscular contusions, the muscle as well as part of the sheath surrounding it gets torn. This results in a longer bleeding time initially, especially if there is no use of ice therapy. The patient usually recovers faster from this type of dead leg, as the blood and fluids can easily flow away from the injury site. Bruising is often present in this type of contusion.

 Metatarsalgia is the name given to pain in the front part of your foot under the heads of your metatarsal bones ( ball of foot, just before toes). It is usually worse when standing or walking etc. and occurs most frequently in the second, third/or fourth metatarsal joints or isolated in the first metatarsal joint. Metatarsalgia usually comes on gradually over some weeks rather than suddenly. The affected area of your foot may also feel tender on palpation by your physiotherapist.
Metatarsalgia is the name given to pain in the front part of your foot under the heads of your metatarsal bones ( ball of foot, just before toes). It is usually worse when standing or walking etc. and occurs most frequently in the second, third/or fourth metatarsal joints or isolated in the first metatarsal joint. Metatarsalgia usually comes on gradually over some weeks rather than suddenly. The affected area of your foot may also feel tender on palpation by your physiotherapist.