 Overtraining syndrome, a common cause of persistent tiredness in sportspeople, seen by physio’s, frequently occurs in athletes who are training for competition or a specific event and train beyond their bodies ability to recover. Athletes often exercise longer and harder so that they can improve. However without adequate rest, recovery and nutrition, these training regimens can backfire, actually decreasing performance. Proper training and conditioning requires a balance between overload and recovery. The terms overtraining, overreaching, overtraining syndrome, burnout, and staleness have all been associated with overtraining syndrome and need to be clarified. Overtraining is excessive training with inadequate recovery. Overtraining has also been linked to glycogen depletion(Costill et al. 1988) when inadequate refuelling of muscles glycogen occurs due to low carbohydrate intake. The sooner carbohydrate is consumed following a bout of exercise, the more effective the replenishment of glycogen stores. Adequate quality protein intake would also be important in the case of strength athletes to help protect against overtraining syndrome. Sufficient iron intake is important for endurance athletes especially women.
Overtraining syndrome, a common cause of persistent tiredness in sportspeople, seen by physio’s, frequently occurs in athletes who are training for competition or a specific event and train beyond their bodies ability to recover. Athletes often exercise longer and harder so that they can improve. However without adequate rest, recovery and nutrition, these training regimens can backfire, actually decreasing performance. Proper training and conditioning requires a balance between overload and recovery. The terms overtraining, overreaching, overtraining syndrome, burnout, and staleness have all been associated with overtraining syndrome and need to be clarified. Overtraining is excessive training with inadequate recovery. Overtraining has also been linked to glycogen depletion(Costill et al. 1988) when inadequate refuelling of muscles glycogen occurs due to low carbohydrate intake. The sooner carbohydrate is consumed following a bout of exercise, the more effective the replenishment of glycogen stores. Adequate quality protein intake would also be important in the case of strength athletes to help protect against overtraining syndrome. Sufficient iron intake is important for endurance athletes especially women.
The term overreaching describes similar symptoms(fatigue, performance decrements, mood state
changes) but is generally of a more transitory nature and is often utilised by sportspeople/coaches
during a typical training cycle to enhance performance. Intense training, in the short term can result
in a decline in performance; however when incorporated with periods of recovery, a
super-compensation effect may occur, with the sportsperson exhibiting enhanced performance
when compared with baseline level (Halson and Jeukendrup, 2004). Overtraining syndrome
develops when there is failed adaptation to overload training due to inadequate regeneration.
Unfortunately , many sportspeople and coaches, especially at amateur level, react to impaired
performance by increasing the intensity of training. This leads to further impairment of
performance, which may , in turn, result in the sportsperson increasing training even further. A
vicious cycle develops which leads overtraining syndrome.
Changes within the central nervous system seem to play an important role in the development of
chronic fatigue and many of the other common signs and symptoms that are frequently seen in
overtraining syndrome, such as disrupted sleep, changes in appetite and weight, irritability, impaired
concentration, decreased motivation, and depressed mood. It has been suggested that alterations in
levels of brain neurotransmitters(e.g. a reduction in serotonin levels) and an increased release of
inflammatory mediators(e.g. cytokines) are important factors in the development of overtraining
syndrome(Anish, 2005). Many of the signs and symptoms that characterize overtraining syndrome are remarkably similar to those of clinical depression. Unfortunately, no single test can detect overtraining in the sportsperson. Probably the simplest and most effective means of monitoring overtraining is self analysis by sportspeople themselves. Daily documentation should include sources and ratings of stress, fatigue, muscle soreness, quality of sleep, irritability, and perceived exertion during training or standardized exercise.
Blood parameters such as red and white blood cell counts, haemoglobin, hematocrit, urea, and
ammonia are usually normal during overtraining. Changes in exercise blood lactate concentration
and blood lactate threshold however have been shown to be good indicators of overtraining but are
influenced by many other factors and are probably only useful if assessed repeatedly.
The initial symptom of the overtraining syndrome is usually fatigue but in time, other symptoms
develop.(Mackinnon and Hooper, 2000) Indicators of overtraining include; decreased performance
despite continued training, persistent fatigue, increased early morning heart rate or resting blood
pressure, frequent illnesses such as upper respiratory tract infections, persistent muscle soreness,
loss of body mass, mood changes, loss of appetite, sleep disturbance, high self-reported stress
levels, irritability, depression , decreased maximal heart rate. Overtraining syndrome can also leave
an athlete more susceptible to injury.
Deep tissue massage and injury prevention advice is where or physiotherapists come in. Feel free to set up an appointment at our Tralee clinic to discuss things. For more details click here.
REFERENCES
Mackinnon, L.T., Hooper, S.L. Overtraining and overrreaching: causes, effects, and prevention. In :
Garret, W.E., Kirkendall, D.T., eds. Exercise and Sports Science. Philadelphia : Lippincott, William &
Wilkins, 2000.


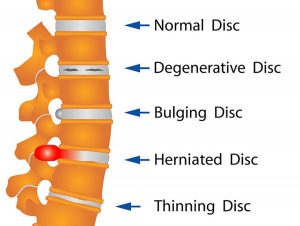 Your spine is made up of lots of bones called vertebrae and discs stacked on top of one another, forming the spinal canal. The nerves of the spinal cord run down the length of the spinal canal. The discs in act like shock absorbers between the vertebrae. These discs are made of two components: a softer center (called nucleus pulposus) surrounded by a tough elastic-like band (called annulus fibrosus). A bulging disc is like a squashed jam doughnut before the jam bursts out. The disc sags and looks like it is bulging outward. With a herniated disc, the outer covering of the disc has a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal. It is like the jam leaking out from the inside of a squashed jam doughnut.
Your spine is made up of lots of bones called vertebrae and discs stacked on top of one another, forming the spinal canal. The nerves of the spinal cord run down the length of the spinal canal. The discs in act like shock absorbers between the vertebrae. These discs are made of two components: a softer center (called nucleus pulposus) surrounded by a tough elastic-like band (called annulus fibrosus). A bulging disc is like a squashed jam doughnut before the jam bursts out. The disc sags and looks like it is bulging outward. With a herniated disc, the outer covering of the disc has a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal. It is like the jam leaking out from the inside of a squashed jam doughnut. Posterior ankle impingement is a condition characterised by tissue damage at the back of
Posterior ankle impingement is a condition characterised by tissue damage at the back of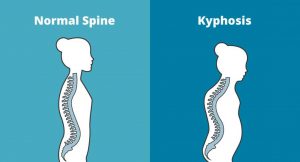 Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is more common in older people. Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time. Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfigurment. Treatment for kyphosis depends on your age, and both the cause and the effects of the curvature.
Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is more common in older people. Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time. Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfigurment. Treatment for kyphosis depends on your age, and both the cause and the effects of the curvature.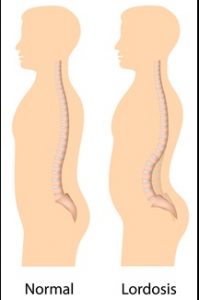 Some curvature in the lower back is normal. However, if your curve arches too far inward, it’s called lordosis, or swayback. Lordosis can affect your lower back and/or neck. The condition can lead to excess pressure on the spine, causing pain and discomfort. It can affect your ability to move if it’s severe and left untreated. Treatment of lordosis depends on how serious the curve is and how you got lordosis. There’s little medical concern if your lower back curve reverses itself when you bend forward. You can probably manage your condition with physical therapy and daily exercises.
Some curvature in the lower back is normal. However, if your curve arches too far inward, it’s called lordosis, or swayback. Lordosis can affect your lower back and/or neck. The condition can lead to excess pressure on the spine, causing pain and discomfort. It can affect your ability to move if it’s severe and left untreated. Treatment of lordosis depends on how serious the curve is and how you got lordosis. There’s little medical concern if your lower back curve reverses itself when you bend forward. You can probably manage your condition with physical therapy and daily exercises. Scoliosis is a medical condition in which a person’s spine curves sideways, usually in an “S” or “C” shape. In some, the degree of curvature remains stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, however severe cases can interfere with breathing. The cause of most cases is unknown, but is believed to involve a combination of genetic and environmental factors. Diagnosis is confirmed by Xray. Treatment depends on the degree of curve, location, and cause.
Scoliosis is a medical condition in which a person’s spine curves sideways, usually in an “S” or “C” shape. In some, the degree of curvature remains stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, however severe cases can interfere with breathing. The cause of most cases is unknown, but is believed to involve a combination of genetic and environmental factors. Diagnosis is confirmed by Xray. Treatment depends on the degree of curve, location, and cause. Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just your joints. It is an autoimmune disease occurring when your immune system mistakenly attacks the synovium , the lining of the membranes that surround your joints. The resulting inflammation causes the synovium to thicken, eventually destroying the cartilage and bone within the joint. The tendons and ligaments holding the joint together also weaken and stretch. Gradually, the joint loses its shape and alignment.
Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just your joints. It is an autoimmune disease occurring when your immune system mistakenly attacks the synovium , the lining of the membranes that surround your joints. The resulting inflammation causes the synovium to thicken, eventually destroying the cartilage and bone within the joint. The tendons and ligaments holding the joint together also weaken and stretch. Gradually, the joint loses its shape and alignment. Natural Anti-inflammatories
Natural Anti-inflammatories
 When somebody first presents in clinic with a muscle injury, it is important to first determine whether it is a muscle spasm or a tear. A spasm/cramp can often be worked out in a session with deep tissue massage and maybe some dry needling and stretching, allowing almost immediate turn to training. A muscle tear takes much longer to recover from, the length of time greatly depending on the degree of tearing. Treatment takes longer and a rehabilitation program is also essential. A muscle spasm is caused by an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time.
When somebody first presents in clinic with a muscle injury, it is important to first determine whether it is a muscle spasm or a tear. A spasm/cramp can often be worked out in a session with deep tissue massage and maybe some dry needling and stretching, allowing almost immediate turn to training. A muscle tear takes much longer to recover from, the length of time greatly depending on the degree of tearing. Treatment takes longer and a rehabilitation program is also essential. A muscle spasm is caused by an involuntary contraction of that muscle. It is usually sudden, can cause significant pain and can limit the use of the muscle for a short period of time. One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.
One of the primary symptoms when a lumbar facet joint locks is an increase in pain on extension of the lower back. Basically there is more pain when you try and straighten up your lower back or lean back on it. This position loads pressure on the locked lumbar facet joints. Usually with this type of injury there is pain relief to a certain extent when a person bends forward. The reason for this is that forward flexion decompresses the facet joint articulations, releasing some of the pressure on the joints and hence the associated pain. There can be nerve irritation with this injury but it is usually more general and not as severe as with discogenic pain.