 Recently in Ireland, people are paying thousands of euro for procedures advertised as ” stem cell treatment ”, for conditions such as osteoarthritis. These treatments are not covered by health insurance companies etc. They often use the term ”stem cell treatment”, for a process that bears little if any resemblance to what stem cell therapy actually is. Below is a summary of an article written by an orthopedic surgeon outlining the limitations of stem cell therapy as it presently stands. Before you part with your money for one of these treatments, have a read of it, discuss it with your doctor and do your research.
Recently in Ireland, people are paying thousands of euro for procedures advertised as ” stem cell treatment ”, for conditions such as osteoarthritis. These treatments are not covered by health insurance companies etc. They often use the term ”stem cell treatment”, for a process that bears little if any resemblance to what stem cell therapy actually is. Below is a summary of an article written by an orthopedic surgeon outlining the limitations of stem cell therapy as it presently stands. Before you part with your money for one of these treatments, have a read of it, discuss it with your doctor and do your research.
Below is a summary of an article written by Mark Miller, Professor of Orthopedic Surgery, University of Virginia, ”Stem cell treatment for arthritic knees is unproven, expensive and potentially dangerous”
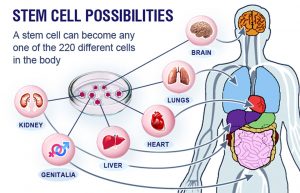
Stem cells are “uncommitted” cells that are, at least theoretically, capable of becoming any type of cell – skin, heart, kidney or even knee cartilage cells. Stem cells can come from fetal tissue, including products of in-vitro fertilization as well as placenta and umbilical cord tissue. They can also come from a patient’s own “hidden” adult stem cells, which are most often harvested from bone marrow and fat. The potential for using these cells in medicine is tremendous.
The truth
Unfortunately, the excitement about stem cells has outpaced the science. In addition, due to the ethical issues associated with the use of fetal tissue, the U.S. Food and Drug Administration has severely restricted its use and obtaining an abundant source of concentrated stem cells can be difficult.
In orthopedics, researchers have proposed using stem cells for the treatment of joint/cartilage damage. This includes osteoarthritis. Osteoarthritis often results in the need for joint replacement surgery. Stem cell injections are now being promoted as a potential way of avoiding the need joint replacement, by ”regenerating” the cartilage. Unfortunately, current technology and regulatory issues make obtaining and concentrating true stem cells a challenge, and encouraging them to become and remain cartilage cells and nothing else is even more difficult.
The problem with stem cells is that these cells can continue to evolve; they may not stop development at the cartilage cell phase. They may continue to differentiate into bone cells. This would make the joint even worse because bone creates a rough surface adjacent to the smooth articular cartilage. Bone is actually the end result of arthritis.
According to the American Association of Hip and Knee Surgeons, there are no proven medications or therapies that can delay or reverse the progressive joint destruction that occurs with osteoarthritis.
Many patients have paid out thousands of dollars for ”so-called stem cell treatment” only to later discover that they were scammed. Any positive effects of current stem cell treatment are likely not the result of the actual cells themselves but something else.
Alternatives to stem cell treatment
Depending on the cause and severity of their joint pain, patients have treatment options that range from physical therapy, to injections of various medications, to surgery. All have pros and cons; steroid injections can provide quick but short-lived pain relief, while a knee replacement can provide a permanent solution but also requires months of rehabilitation. Doctors need to help patients make the choice that best fits their particular needs.
Physiotherapists Tralee phone 086-7700191
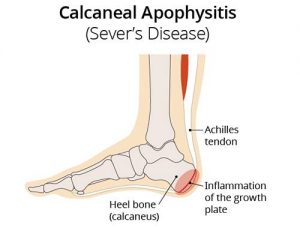 Sever’s disease (also known as calcaneal apophysitis) is a type of bone injury in kids whre the growth plate on the lower back part of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and painful. The reason for this is that the heel bone grows faster than the ligaments in the leg. As a result, muscles and tendons can become very tight and overstretched in children who are going through growth spurts. Sever’s disease occurs as a result of repetitive stress on the Achilles tendon. Over time, constant pressure on the already tight achilles tendon can damage the growth plate, causing children. Symptoms of Severs disease include pain and inflammation. This is why it is more common in physically active.
Sever’s disease (also known as calcaneal apophysitis) is a type of bone injury in kids whre the growth plate on the lower back part of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and painful. The reason for this is that the heel bone grows faster than the ligaments in the leg. As a result, muscles and tendons can become very tight and overstretched in children who are going through growth spurts. Sever’s disease occurs as a result of repetitive stress on the Achilles tendon. Over time, constant pressure on the already tight achilles tendon can damage the growth plate, causing children. Symptoms of Severs disease include pain and inflammation. This is why it is more common in physically active.