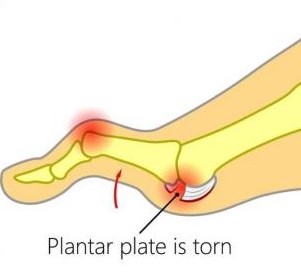
Plantar plate injuries are easily missed, probably because a lot of people don’t know what the plantar plate is. Quite they are diagnosed under the general term metatarsalgia. The plantar plate is a deep fibrocartilaginous structure that originates from the metatarsal head and attaches to the proximal phalanx through the joint capsule within the forefoot. Its role is to help stabilize the metatarsophalangeal joints (MTPJ), along with a couple of other structures. The plantar plate also acts as an attachment site for the plantar fascia, so if you load the foot, the medial arch lengthens, the plantar fascia tightens, this engages the plantar plate to plantarflex the proximal phalanx until the toe reaches the ground. This is a simplification of a complex process and is commonly known as the The ‘reversed’ windlass mechanism (with weight-bearing the longitudinal arch flattens, the foot lengthens, the plantar fascia tightens, the proximal phalanx becomes plantarflexed and the mechanism comes to a stop when the proximal phalanx presses against the ground).
What causes a plantar plate injury and how common are they?
There are many contributing factors. The first is any activity that exposes the MTPJ to repetitive and excessive dorsiflexion, so think about jumping and running especially in forefoot runners. There are a few biomechanical conditions that increase the load through the plantar plate such as hallux valgus (bunions). As the function through the 1st MTPJ(big toe) is reduced, then we get what is known as low gear propulsion and increased loading through lesser MTPJs, typically the 2nd, 1st, then 3rd and so on. Another condition like having say an irregular metatarsal length, for example, if you have a long 3rd metatarsal, can expose the plantar plate to increased load, as can external factors like high heels. Basically anything that will result in excessive dorsiflexion or ground reaction forces at the MTPJs may increase plantar plate loading.
How does a plantar plate injury present?..
- The patient will complain of pain on the dorsal and plantar aspects of the MTPJ, usually described as an ache or bruising.
- Mild oedema may be present along with an episode of trauma, however, trauma is not essential as plantar plate injuries are typically a chronic overuse injury
- Weight-bearing activities increase pain – especially dancing, forefoot running, barefoot walking, etc
- Rest /non-weight bearing reduces pain.
- High heels or flexible footwear increases pain
- Reduced plantarflexion strength – The ‘Digital Purchase’ test
- A quick way to do this, put a piece of paper under the apex of the affected toe and ask the patient to try and stop you pulling the paper away, in a plantar plate injury you will notice the paper is pulled away much more easily.
- Pain, oedema and positive Digital Lachmans (Anterior Draw) / Vertical Stress.
- Floating toe, if late-stage hammertoe, or Churchill sign may be present.
Diagnosis of plantar plate injuries
Digital Lachmans / Vertical Stress Test (Fig 1)
Same style of test to assess ACL tears, helps to assess the integrity of the plantar plate, it is quick, easy and a simple test to perform. Stabilise the head of the metatarsal with one hand, using the other hand stabilise the base of the proximal phalanx, apply a vertical force, we are looking for pain and any translocation, it is important to remember this is different from dorsiflexion of the digit.

There are 2 scoring systems one by Thompson and Hamilton and the other Yu and Judge
Thompson and Hamilton
- Stage 0, there is no dorsal translocation present of the proximal phalanx.
- Stage 1 the base of the phalanx, will not dislocate, however, may sublux
- Stage 2 the base of the phalanx can be dislocated.
- Stage 3 the phalanx base is in a fixed dislocated position
Yu and Judge
- Stage 1 mild odema on the plantar MTPJ with dorsal odema often present as well. Tenderness is present on palpation, however no anatomical malalignment.
- Stage 2 moderate odema is present with a noticeable deviation.
- Stage 3 odema present around the entire MTPJ with deviation and possible dislocation/subluxation, the odema will reduce however the deformities will remain.
I think the best way to describe the 2 different methods of testing, would be that the Thompson and Hamilton test best describes the integrity of the plantar plate at any given time, whereas the Yu and Judge test describes different stages based on clinical findings on the time of examination.
MRIs, X-rays and Ultrasound
There is still some debate as to whether an MRI scan or ultrasound scan is best for detecting plantar plate injuries. As we know ultrasound is cheaper, however, it is user-dependent, whereas MRI scan is more expensive but we can also get an overall picture of the structures within that area as well. X-ray in weight-bearing (lateral or oblique views) will show subluxation dorsally of the proximal phalanx on the metatarsal head, an anterior-posterior view will show a transverse deformity as well. An x-ray will also rule out other bony pathologies.12
Treatment of plantar plate injuries
The aim of treatments, like most musculoskeletal pathologies, is about managing the load. Essentially we want to try and reduce the ground reaction forces under the affected metatarsal head and reduce the plantarflexion moment of the metatarsal and the dorsiflexion of the phalanx.
Treatment protocols include
- No barefoot walking/activity modification
- Footwear advice / Air cast boot – we want to look at using a stiff-soled shoe, or reducing the heel height of a shoe, so footwear like high heels and the flexible minimalist type shoes tend to aggravate a plantar plate injury, the same goes for open-toe shoes and flip-flops, as you must claw your toes to keep these on which again increases the ground reaction force underneath the metatarsal.
- Stretching / Strengthening – thinking about the mechanics of the foot, if there is tightness within the calf muscles, in turn, could result in early and increased loading through the forefoot, and if you are unable to get adequate dorsiflexion due to calf tightness, then the foot may pronate to compensate for this, which in turn could increase the loading through the lesser MTPJ’s. It is important also to work on strengthening the muscles within the foot.
- Strapping can be very helpful in reducing pain, using a rigid zinc oxide tape and pulling the toe into a plantarflexed position to help offload a plantar plate (Fig 2).

Orthotics
Orthotics can be a useful way to help offload the affected plantar plate. One of the best ways to treat Plantar Plate Injures with or without surgery is using an orthotic device that places the pressure into the archway and off of the ball of the foot. If manufactured and molded correctly, they can keep the tension off the injury and pressure when standing and walking. Combining the orthoses with taping and footwear advice can be quite an effective way of offloading the affected plantar plate, whilst the patient reduces sporting activities.
Steroid injections
Steroid injections can be tried , however repeated intra-articular injections has been shown to result in dislocation of the MTPJ. It has also been suggested that injections into a ligament resulted in destruction of fibrocytes and reduction in tensile strength for up to 1 year which in turn may result in further damage a possible rupture.
A recent case study showing a patient with a plantar plate tear was managed using conservative measures, consisting of taping, activity modification and the use of a Darco boot over a 6 month period, and progressing to stiffed shoe and orthoses and stopped taping. At the 1 year mark, the patient was pain-free with no toe deformity, and on MRI the plantar plate has healed.
So what’s my treatment plan?
- No barefoot walking for 6 weeks (minimum)
- To wear stiff-soled shoes
- Strapping of digit changing every 72 hours
- Activity modification
- Orthoses as described as above, plus any other modifications required
- Stretching and Strength work – Distal and proximal
If conservative measures fail, then it may require referral to a surgeon.
Physiotherapist in Tralee. Ring to discuss your condition, to get a second opinion or to make an appointment. Click here for website.

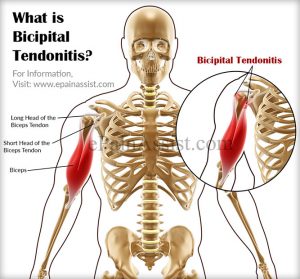 Bicipital tendonitis is a common cause of shoulder pain, often developing in people who perform repetitive, overhead movements. Biceps tendinitis develops over time, the pain being located at the front of the shoulder. The biceps muscle has two parts referred to as the long head and the short head. The tendon of the long head of the biceps is most commonly implicated with tendonitis. When this tendon is subjected to repetitive stresses, it can become irritated, swollen, and painful.This occurs where the tendon sits within the bicipital groove at the top of the humerus under the transverse ligament before it becomes part of the shoulder joint capsule.
Bicipital tendonitis is a common cause of shoulder pain, often developing in people who perform repetitive, overhead movements. Biceps tendinitis develops over time, the pain being located at the front of the shoulder. The biceps muscle has two parts referred to as the long head and the short head. The tendon of the long head of the biceps is most commonly implicated with tendonitis. When this tendon is subjected to repetitive stresses, it can become irritated, swollen, and painful.This occurs where the tendon sits within the bicipital groove at the top of the humerus under the transverse ligament before it becomes part of the shoulder joint capsule.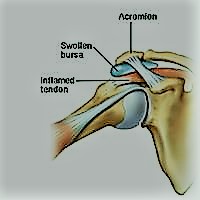 Sub-acromial bursitis is a common cause of shoulder pain that is usually related to impingement of the bursa between the supraspinatus muscle tendon and the acromion bone(see diagram). Bursae(single = bursa) are fluid-filled sacs that help reduce friction wherever tendons move under or over bone. The Supraspinatus muscle runs along the top of the shoulder blade and inserts via the tendon onto the top of the arm(humerus bone). This muscle is used to lift the arm up sideways . Above the supraspinatus tendon and under the acromion there is a bursa. When this bursa gets inflamed and swollen it can become trapped under the acromium bone of the shoulder causing pain and inflammation.
Sub-acromial bursitis is a common cause of shoulder pain that is usually related to impingement of the bursa between the supraspinatus muscle tendon and the acromion bone(see diagram). Bursae(single = bursa) are fluid-filled sacs that help reduce friction wherever tendons move under or over bone. The Supraspinatus muscle runs along the top of the shoulder blade and inserts via the tendon onto the top of the arm(humerus bone). This muscle is used to lift the arm up sideways . Above the supraspinatus tendon and under the acromion there is a bursa. When this bursa gets inflamed and swollen it can become trapped under the acromium bone of the shoulder causing pain and inflammation.