 Spinal manipulation is a technique where practitioners use their hands or a device to apply a controlled thrust to a joint of your spine. The amount of force can vary, but the thrust moves the joint more than it would on its own. It is designed to relieve pressure on joints, reduce inflammation, and improve nerve function. It’s often used to treat back, neck, shoulder, and headache pain in combination with other treatments i.e. deep tissue massage, electrotherapy, rehabilitation exercises. The common goal of most spinal manipulations is to restore or to enhance joint function, with the general goals of resolving joint inflammation and reducing pain.
Spinal manipulation is a technique where practitioners use their hands or a device to apply a controlled thrust to a joint of your spine. The amount of force can vary, but the thrust moves the joint more than it would on its own. It is designed to relieve pressure on joints, reduce inflammation, and improve nerve function. It’s often used to treat back, neck, shoulder, and headache pain in combination with other treatments i.e. deep tissue massage, electrotherapy, rehabilitation exercises. The common goal of most spinal manipulations is to restore or to enhance joint function, with the general goals of resolving joint inflammation and reducing pain.
Spinal Manipulation Techniques
Physiotherapists and osteopaths adapt treatment plans to meet the specific needs of each patient. Some of these treatment plans involve some forceful and less forceful spinal adjustment techniques during the same visit or over the course of treatment .
Spinal Manipulation (High-Velocity Low-Amplitude Thrust)
The most frequently used technique, spinal manipulation, is the traditional high-velocity low-amplitude (HVLA) thrust. The manipulation often results in an audible “pop,” as physiotherapists use their hands to apply a controlled sudden force to a joint while the body is positioned in a specific way.
Is the audible pop necessary ?
Spinal Mobilization (Low-Force / Gentle Techniques)
Some patients and/or clinicians prefer mild spinal mobilization techniques that do not involve twisting of the body or a forceful thrust.The goal of spinal mobilization is the same as HVLA spinal manipulation – to restore or to enhance joint function. However, unlike HVLA spinal manipulation, slow movement, usually to a firm endpoint of joint movement, is used to mobilize the joint.
Physiotherapists may choose spinal mobilization for certain patients for a variety of reasons, such as:
- Patient preference – certain patients prefer spinal mobilization over spinal manipulation.
- Obesity can make the positioning of the patient and the manipulation procedures challenging for both the provider as well as the patient, which might favor a low force technique.
- Patients with sensitive nervous systems may benefit from gentle mobilization techniques to keep the body from overreacting and causing reactive muscle spasms.
- Patients with some conditions may be contraindicated for spinal manipulation, such as possibly patients with advanced osteoporosis, bone pathology, some forms of deformity, and certain types of inflammatory arthritis.
- Physiotherapists may choose spinal mobilization for patients when they are in the acute stage of their condition and in severe pain.
- Obesity can make the positioning of the patient and the manipulation procedures challenging for both the provider as well as the patient, which might favor a low force technique.
See video below demonstrating spinal manipulation

 Posterior ankle impingement is a condition characterised by tissue damage at the back of
Posterior ankle impingement is a condition characterised by tissue damage at the back of
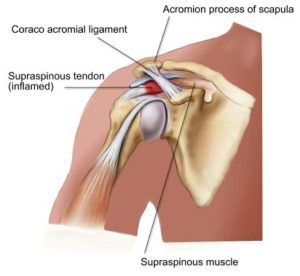 Shoulder impingement is a very common cause of shoulder pain, where a supraspinatus tendon inside the shoulder rubs or catches on nearby tissue and/or bone(acromium) as you lift your arm.
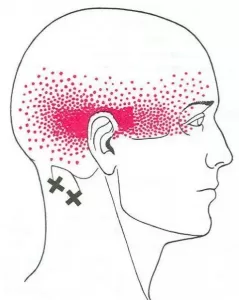
Shoulder impingement is a very common cause of shoulder pain, where a supraspinatus tendon inside the shoulder rubs or catches on nearby tissue and/or bone(acromium) as you lift your arm. 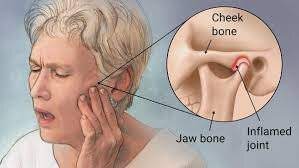 The temporomandibular joint works as a combination of hinge and sliding actions. It connects the jawbone to the skull on each side of the face. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth. Temporomandibular joint disorder (TMJD) can cause pain in your jaw joint and in the muscles that control jaw movement.
The temporomandibular joint works as a combination of hinge and sliding actions. It connects the jawbone to the skull on each side of the face. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth. Temporomandibular joint disorder (TMJD) can cause pain in your jaw joint and in the muscles that control jaw movement.